Written by: Louise C. Miller, R.T.(R)(M)(ARRT), CRT(M), FSBI, FNCBC, Director of Education
This blog article is the first of a two part series on challenging patients. This month addresses positioning challenges: body habitus, physical limitations, breast size etc. Part 2 will address other challenges: developmental disabilities, manifestations of anxiety, previous bad experiences with mammography/the technologist, victims of abuse, etc. These recommendations have been presented in many lectures and publications for the ACR/SBI, are based on my experience and from what I have learned from breast imaging professionals, for which I am most grateful. Obviously nothing works for everyone all the time, but I am hopeful that these BLOGS will encourage additional conversations between technologists and radiologists, as we strive to do our best to provide quality patient care while realizing that there are limitations to what we can reasonably accomplish.
In my 35+ years of teaching mammography and trying to improve and standardize positioning techniques, the question I get asked the most is: How do you get ACR “perfect” images on every patient? The answer: You don’t... and you can’t, due to patient limitations. All good radiologists should understand this. There is data (1) to support this which shows, even after an ACR positioning training, only 67% would meet ACR criteria, let alone be an image that you would send in for accreditation, which is supposed to be a representation of your BEST work.
I also have had the opportunity to write a 3-part article for radiologists that was published in the Society of Breast Imaging (SBI) Newsletter titled: What Every Technologist Would Like Their Radiologist to Know (2, 3 4), in which I attempted to represent the challenges that mammography technologists face daily. Both articles can be found on the Resources page of our website. I encourage you to share these articles with your radiologists and start a conversation so they can better understand the challenges you experience and therefore establish realistic expectations regarding positioning standards.
I would also like to remind you of your experience in general radiology.
Remember the portable CXRs we did in the ICUs. We would struggle to get the patient seated (somewhat) upright, struggle to place the cassette behind them, try to encourage them to keep their chin up so it would not be superimposed over the lung field. All the nurses ran when you yelled out “X-RAY”, so no one was there to help hold the patient. You get back to the department, develop the film (yep, that was in the “olden days” LOL 😊,) only to find that the entire mandible and head obscured visualization of a portion of the apecies of the lungs! (Figure 1) We would not freak out. We did our best. You would not be going back to the ICU and repeating the image over and over trying to get it to look like a “normal” patient/CXR.
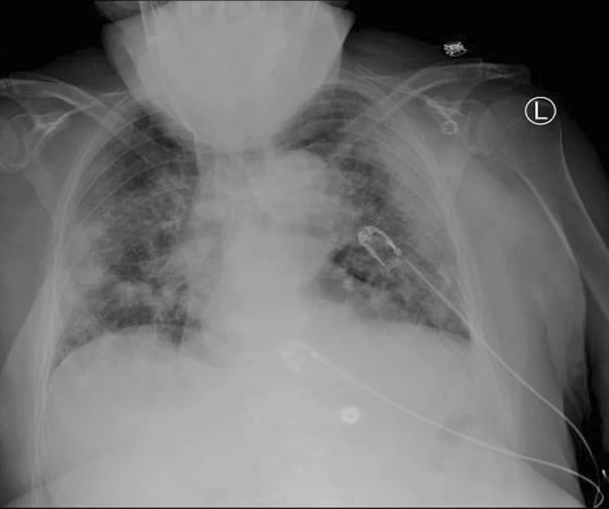
Figure 1
Let me give you another example...
You have a patient who has severe arthritis of his/her hand. (Figure 2) You could never, no matter how many positioning skills you possess, years of experience or “tricks” you know, make that hand look like a “normal” hand. (Figure 3)

Figure 2 Figure 3
So why do we have such different expectations for mammography?
Let’s say you have a patient who is in a wheelchair, she cannot stand and the arms cannot be removed from the chair. The patient also is on oxygen, is kyphotic, had recent open heart surgery and a frozen shoulder. Okay, maybe I am exaggerating a bit (but we have all dealt with any/all of these “combos”). My point is that we could never get images that look comparable to a patient who presents none of the same challenges. Please understand that I would never advocate turning in “substandard” images. However, you can only do so much under certain circumstances. The most important thing to remember is that you document the patient's limitations clearly for the radiologist and in appropriate terminology, so that they will understand the reason for the compromised image. It is also recommended that that radiologist will include this information in the report so that this is part of the patient’s medical record moving forward.
With that said, here are some of the things I have found that might help you get better, not perfect, images on some of these patients. I also always try to do the standard views first, to show the radiologist I made the effort, and then add additional views in an attempt to demonstrate more breast tissue.
EXTREMELY LARGE BREASTS
If you have to mosaic or tile the breast, I always try to include the lateral breast on the CC views first. If I can, then I do one CV view to include the medial breast tissue of each breast; this will save you an extra image. However, your radiologist should be in agreement that they feel this is an acceptable alternative to doing medial CCs on each breast. Sometimes you will have to do an anterior CC view of very large breasts.
For the MLOs, I always use a lower degree of angulation. I find that 40 degrees works well. The lesser degree will counteract the effect of gravity caused by the weight of the breast and will help support the breast and the patient. You may also need to mosaic/tile the breast, especially if the patient has a prominent axillary fat pad which may prohibit adequate compression of the anterior breast.
Three Additional Tips for the MLO (Extremely Large Breasts):
- Push up the breast higher than you think you need to, even if you get a crease in the axilla. It will probably “fall out” as compression is applied. It is also far more important to visualize glandular breast tissue in the anterior breast. Also, DBT will help the radiologist scroll through the fold.
- Don’t let go until the breast is completely compressed. I find that most techs let go too soon, which will cause the breast to drop/droop (the dreaded “camel’s nose”). Our goal is to keep the nipple as close as we can to perpendicular to the chest wall to overcome superimposition of glandular breast tissue.
- Have the patient lift and flatten her contralateral (opposite) breast. You won’t believe how great this works in opening the IMF and eliminating folds in this area.
NOTE: I do not promote having the patient bend or lean in for the CC or MLO on patients with large breasts or other patients in general. There may be times that this is necessary, but in general practice, I would not recommend this as it could mean the exclusion of inferior breast tissue on both views.
EXTREMELY SMALL BREASTS/LARGE FLACCID BREASTS
One of the biggest challenges here is to try to keep the breast in place without the compression paddle hitting your hand(s). If your machine has a half-paddle, use that! You could also position from behind the patient (sit her down if necessary) and use the Implant Displacement (ID) Technique that is posted on our website.
PATIENTS IN WHEELCHAIRS
The first thing I do is to remove the arms of the wheelchair, if that is possible. I also move the foot supports out of the way to make it easier to position the “whole patient”. I then try to get the patient as upright as possible in the chair. Many times they slump down and this (maybe combined with kyphosis!) makes it much harder to position the patient/breast. I also try to get her hips and buttocks as far forward in the wheelchair as possible, obviously taking care that her safety is not compromised (a consideration in removing the arms of the wheelchair as well). You can use pillows or sponges to help keep her in this position.
For the CCs, I may do the “lordotic” CCs as described above. This is one of the few times when I will have the patient lean forward for the CCs. For the MLOs, I bring the wheelchair in at a 45 degree angle. (Figure 4a) This helps to better image the axilla and anterior breast. You should remember that it is very difficult to visualize the IMF on these patients, especially if they have prominent abdomens, so adjust your expectations accordingly and be sure to document the patient limitations on the history sheet.

Figure 4a Figure 4b
LIMITED ROM/SHOULDER PROBLEMS
Limited range of motion should not be a problem when positioning for the CCs. For the MLOs, you must access the mobility of the patient and her arm/shoulder before you begin positioning. If she cannot raise her arm up and over the IR, simply lift their axilla over the corner of the IR and allow her arm to hang freely behind the IR.
PROMINENT ABDOMENS
One of the most challenging patient body habitus can be those patients with small breasts and large abdomens. If the abdomen is hard and distended, it makes it very difficult to image the IMF. An additional lower MLO view, focusing on the IMF can be performed. A LM focusing on this area is also an alternative. I do not abduct the hips (have them stick their butt out, as many of you describe) as this could mean the exclusion of posterior, inferior breast tissue. It is also important to note that excessive abdominal tissue will result in additional skin/fat folds. Data shows (5) that in an analysis of all MLOs (all patient body habitus) will demonstrate skins/fat folds in the lower breast on 49% of all MLOs.
OTHER LIMITATIONS/CHALLENGES
Obviously there are numerous other factors that can make positioning more challenging: kyphosis, scoliosis, lordosis, presence of medical devices, partial or full paralyzes, recent surgery(s), stability and balance issues, encapsulated implants, transgender patients, etc. etc. In this blog, I have tried to present some solutions to the “most requested” positioning dilemmas. Future publications, which are in progress, will cover these topics as well as more detailed instructions related to the patient challenges that have been addressed in this blog.
Additional Resources:
- Mammographic Positioning: Evaluation from the View Box
- How to Help Your Technologist - Part 1: The Inframammary Fold: How to Improve Visualization and Reduce Skin/Fat Folds in the Inframammary Fold
- How to Help Your Technologist - Part 2: Not Enough Pectoralis and the Sagging Breast
- How to Help Your Technologist - Part 3: Common Problems with the Craniocaudal View
- Mammography Positioning Standards in the Digital Era: Is the Status Quo Acceptable?