Written by: Louise C. Miller, R.T.(R)(M)(ARRT), CRT(M), FSBI, FNCBC, Director of Education
Tangential Views and Triangulation... They can be powerful tools in mammography, but most techs are a bit nervous when thinking about WHY and HOW to do them that they have become perhaps the most “mysterious” things related to positioning. But, don’t worry! No need to be afraid any longer. We have figured out some pretty easy ways to think about it and provide some clues that will help answer the questions that often accompany these two concepts.
Tangential Views
Labeling Code: "TAN" (preceded by laterality L or R)
WHY?
Tangential views are done for one of two specific reasons:
- To prove the existence of dermal calcifications
- To better visualize a subcutaneous mass that would otherwise be superimposed on dense, glandular breast tissue
The purpose is to take an area of concern (skin ca# or mass) and project it over radiolucent fat (directly under the skin) to better analyze the location of calcifications and/or the characteristics of those calcifications or masses.
HOW?
As you cannot see or palpate skin calcifications, we must first perform a “skin localization” to determine their exact location. This must be done prior to performing a TAN view.
I learned this from Dr. Daniel Kopans several years ago and it made perfect sense. You are going to do exactly the same thing you would do for a needle localization, but instead of the radiologist inserting the needle, you will simply place a BB on the area of concern and then do a TAN view.
Please note: The use of DBT (and ultrasound for masses) has all but eliminated the need for tangential views, but if your radiologist wants you to still do them for skin calcifications, the method is described below.
STEP-BY-STEP GUIDE
Step #1:
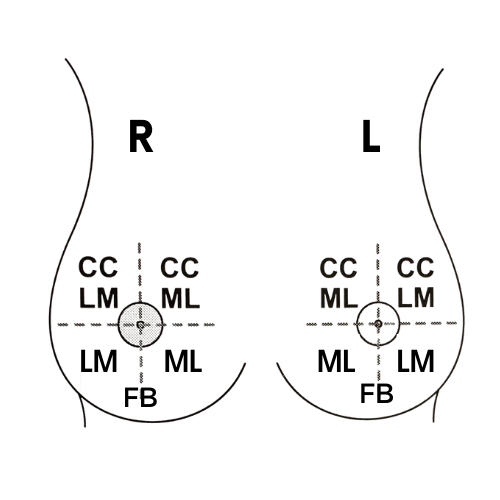
On the breast of interest, determine which quadrant the calcifications are located in. There are only 4 choices: UOQ, UIQ, LIQ and LOQ. This is easy to determine in a matter of minutes by asking yourself the following questions...
- First, look at the MLO or the CC - Are the calcifications in the top part of the breast, which would be indicated by "U" (upper) or the bottom part, which would be indicated by "L" (lower)?
- Next look at the CC only - Are the calcifications in the lateral part of the breast, which would be indicated by "O" (outer) or the medial part of the breast, which would be indicated by "I" (inner).
Step #2:
Engage your biopsy paddle on the machine
Step #3:
Before positioning the patient, set the machine so the automatic compression release feature is OFF. The patient needs to be in compression until you have identified the location of the calcifications.
Step #4:
Using the fenestrated biopsy paddle with alphanumeric coordinates, position the “open/window” portion over the quadrant in which the calcifications were seen and/or over the approximate location where they are seen.
- If they are located in the upper/top of the breast, you will use a CC.
- If they are located in the bottom of the breast, you will use a lateral view. (As shown in the illustration on the right.)
Step #5:
Make exposure and check image to see location of ca# within the biopsy paddle opening.
Step #6:
Using the alphanumeric coordinates, mark the location of the ca# with a BB and then release the compression paddle.
Step #7:
Replace the biopsy paddle with the small compression paddle.
Step #8:
Select the correct view: (R or L) TAN. Then, reinstate auto compression release.
Note: A tangential view is never labelled LMLOTAN, RCCTAN, etc. While the positioning of the machine and patient may look like a CC, MLO or Lateral, it is still labeled "L" or "R" and "TAN" (i.e.: LTAN, RTAN), regardless of the tube angle or patient position.
Step #9:
Turn the breast, patient or tube so that the BB is now in tangent to the beam. (Think of it like a nipple in profile view, with the BB now being the nipple.)
- Another way to do this is to draw an “imaginary line” between the BB and the nipple and then gather the tissue along that “line” and then angle the tube, patient or breast so the line is parallel to the IR.
- Pictures of this can be found in the SBI Newsletter (Click the image on the right.)
Step #10:
Make exposure.
FINAL NOTES...
Dermal calcifications have distinct characteristics. They are usually low density, round and often have a lucent center. Dr. Kopans taught me that skin calcifications may be related to enlarged hair follicles, so this is why we tend to see them within a few centimeters of the skin line, the lower breast and behind the nipple. On the CC, they are commonly seen in the cleavage area. On the MLO, they can be seen in/around the IMF. However, due to superimposition and the stretching of the skin during positioning, they can appear to be anywhere! (Here's another great reference.)