Written by: Sarah Jacobs, BS, R.T.(R)(M)(CT), Breast Imaging Consultant
A few months ago, I was fortunate to spend some time working with a technologist at one of the positioning trainings I was leading. (For the purpose of this story, I’ll refer to this technologist as Amber.)
Amber was quick to pick up on each little tip and trick that I shared with her; I was so pleased at how quickly she was progressing with improving imaging quality. On the last day, I observed Amber discussing the case with another technologist as they were walking towards the Radiologist’s office. The patient was in the clinic for a new palpable lump on her right breast.
| I asked her about the patient’s history with questions like: |
|
Amber responded saying, “We typically don’t ask those questions because our radiologist usually knows that information already.” This was surprising to me, as my role as a mammography technologist has always been to communicate the case to the radiologist by preparing a presentation that answers these questions.
During a recent conversation with Dr. Nathan Groebner, MD, Lead Interpreting Physician at Allina Health’s New Ulm Medical Center, he commented, “Technologist presentations can vary quite a bit, depending on the individual who is presenting.” However, a consistent and concise presentation can assist the radiologist in making a more accurate diagnosis. This method of presenting diagnostic cases to radiologists is something that is often overlooked and should be an integral part of a technologist’s training.
A technologist’s education is focused on mammographic views, protocols, policies and procedures and eventually, radiologist preferences. Diagnostic mammography can produce a significant amount of anxiety for patients, therefore it’s imperative for a tech to be able to present a case with clarity and efficiency.
At the completion of imaging, the technologist is most likely standing outside the door of the reading room or ready to call the offsite radiologist on the phone. At that time, she should be prepared to provide several details that will make presenting the case a more efficient and stress-free experience for everyone.
So, how do I prepare a Diagnostic Presentation?
When acquiring a patient’s history, it is very important that the technologist uses common terminology to obtain relative clinical history. The information acquired can then be translated to appropriate medical terminology when presenting the case (ie: breast pain/mastalgia).
Step 1 – The technologist should determine the reason for the exam – additional views or new concern.
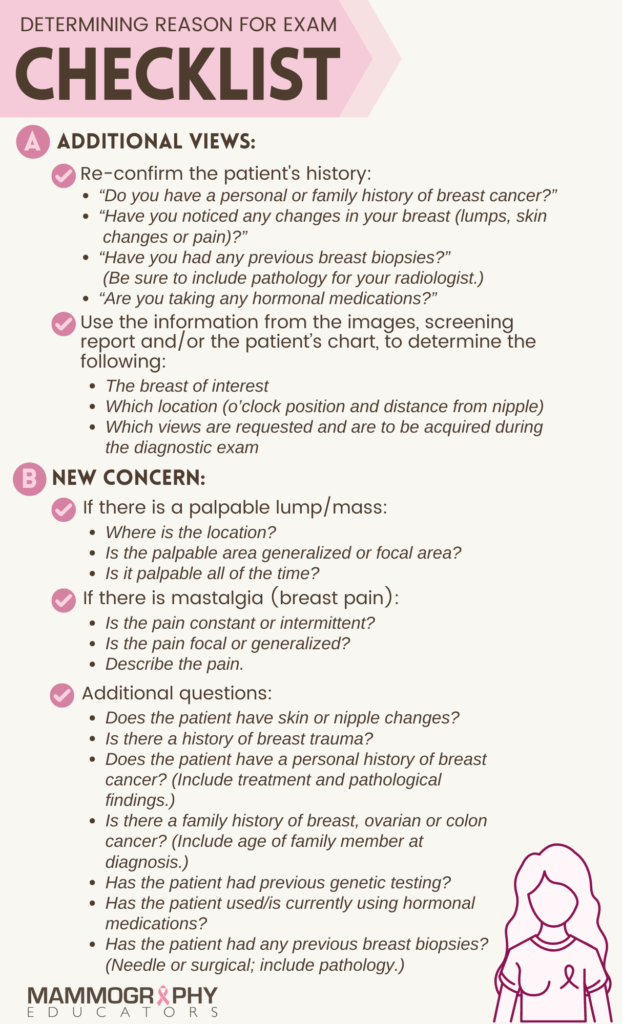
1. ADDITIONAL VIEWS:
If the patient is called back for additional views, the technologist should re-confirm the patient’s history by asking the patient:
- “Do you have a personal or family history of breast cancer?”
- “Have you noticed any changes in your breast (lumps, skin changes or pain)?”
- “Have you had any previous breast biopsies?” (Be sure to include pathology for your radiologist.)
- “Are you taking any hormonal medications?”
The technologist should then use information from the images, screening report and/or the patient’s chart to determine the following:
- The breast of interest
- Which location (o’clock position and distance from nipple)
- Which views are requested and are to be acquired during the diagnostic exam
2. NEW CONCERN:
If the patient is presenting with a new concern, the questions asked during this scenario are slightly different than the history related questions (listed above) that you may ask the patient during a call-back.
When the patient comes in for a new concern, the technologist may ask:
- If there is a palpable lump/mass:
- Where is the location?
- Is the palpable area generalized or focal area?
- Is it palpable all of the time?
- If there is mastalgia (breast pain):
- Is the pain constant or intermittent?
- Is the pain focal or generalized?
- Describe the pain.*
- Does the patient have skin or nipple changes?
- Is there a history of breast trauma?
- Does the patient have a personal history of breast cancer? (Include treatment and pathological findings.)
- Is there a family history of breast, ovarian or colon cancer? (Include age of family member at diagnosis.)
- Has the patient had previous genetic testing?
- Has the patient used/is currently using hormonal medications?
- Has the patient had any previous breast biopsies? (Needle or surgical; include pathology.)
*The questions related to women presenting with breast pain should be specific, as breast pain is a common reason for diagnostic work-ups. According to a study completed in 2014 by the National Library of Medicine, 50% of women studied experience some sort of breast pain(1). Another study from the AJR in February 2020, found that up to 69% of women report regular premenstrual breast pain, and 36% of these women had consulted a health care provider about the pain(2) .
Step 2 – Confidently present the information to the radiologist.
When “presenting” the case to an interpreting physician, it’s important to give information regarding the patient’s history, symptoms and current clinical situation in order to promote efficient and accurate communication that will lead to high quality patient care and safety(3).
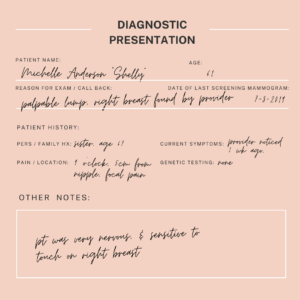
- The presentation should be concise and informative, and usually last no more than 10 seconds. Using a form with this information documented may help you build repetition until you are comfortable with the process of presenting (as shown in the image to the left).
- Do not present “from memory” until you’re comfortable and competent in this process.
- Don’t assume that the physician radiologist already knows everything he or she needs to know about the case you’re bringing to him/her.
- After presenting, allow the radiologist to access and ask any questions he or she may have. If the radiologist has a question that you are unable to answer, volunteer to find the answer whenever possible.
- Any additional information about the patient’s demeanor or mindset may be helpful to present to the radiologist at this time.
- Think critically about the case you’re about to present and don’t be afraid to offer possible solutions that may aide in problem-solving the case.
Effective communication when it comes to diagnostic work-ups extends beyond diagnostic case presentations to the interpreting physician.
Presenting also applies to simple phone calls to let the radiologist know you’re ready for them to come in during a biopsy or other breast procedure. Don’t be afraid to ask the radiologist for feedback after the case has been presented. If he or she has suggestions for improvement, take them as a learning experience. REMEMBER, the radiologist is relying on you, to be their eyes and ears during a diagnostic work-up.
“Having a consistent approach to your presentation will convey the key information, increase the efficiency and accuracy of the workup and lead to better patient care”, says Groebner. Using these simple steps will allow you, as the technologist, to provide accurate information and compassionate care for the patients you serve.
REFERENCES:
- Scurr J, Hedger W, Morris P, Brown N. The prevalence, severity, and impact of breast pain in the general population. Breast J. 2014 Sep-Oct;20(5):508-13. doi: 10.1111/tbj.12305. Epub 2014 Jul 7. PMID: 25041468. https://pubmed.ncbi.nlm.nih.gov/25041468/
- Anna I. Holbrook. Breast Pain, A Common Grievance: Guidance to Radiologists. American Journal of Roentgenology 2020 214:2, 259-264. https://www.ajronline.org/doi/full/10.2214/AJR.19.21923#_i18
- Hadley R, Derenburger D, Patient History: Details, Documentation and Delivery. Society of Breast Imaging Quarterly Newsletter. https://2dr8gzppznj1vs5y82zgbuxh-wpengine.netdna-ssl.com/wp-content/uploads/2020/10/Patient-HX-SBI-Newletter.pdf
NOTE: This blog provides some great information regarding the presentation of diagnostic cases to radiologists. Sarah has included an extensive list of questions and answers that could be relevant to the patient’s workup. However, as individual radiologists may have preferences as to which items/information they prefer to receive, we hope that this blog will provide you with an opportunity to engage in a conversation with your radiologists so you can tailor the case presentation according to their individual/group preferences.


