I have been lucky, over the years, to be invited to speak at some very prestigious breast imaging conferences. I was always impressed, and maybe a bit confused, that every presentation and most every slide had references to at least one, or more scientific studies. I really never thought much about the science of mammography after I memorized and faked my way through the physics part of the registry. (Ugh! It was painful and I still don’t understand what Bremsstrahlung has to do with anything, although I am sure it is important.)

As I grew in my career, I became more and more fascinated with the scientific evidence and studies that were published in medical journals, especially related to breast imaging. I understood that clinical trials done in the 1980s and 1990s set the precedent for the recommended screening guidelines in mammography, but I didn’t understand how that really translated to my everyday work, which was performing mammograms, especially in regards to the positioning component. When you think about it, mammography involves several scientific categories: anatomy, physiology and physics. (There’s that word again!) Rather than just focusing on the “how to” of positioning, (which is what we were all taught), I started thinking of the anatomy and physiology of the breast and how that was demonstrated on my images. But more importantly, if it wasn't demonstrated properly, I could then figure out how to fix my positioning based on my understanding of anatomy. My go-to solution in the past...if I didn't get pec muscle down to the PNL on the MLO view, I would either: a) change the angle (up or down, basically a coin toss), b) adjust the height of the bucky (remember, it was in the "olden days", before digital and IRs), or c) "push and shove" the patient a little and hope for the best. If it didn’t get better, I would repeat a, b and/or c. If it still didn’t get better, I would write on the history sheet, “Patient too difficult to position.”
I started to realize that when we over-rotate the wrist for an oblique view, we can usually correct it before taking the image, analyzing the position of the anatomy of the wrist using our visual and palpation skills. Let’s say you're thinking you got it right - You took the image, but the oblique is over rotated. We then know how to fix positioning based on our understanding of anatomy - move the wrist more medially or laterally depending on the correction we needed to make. We do this with spines, skull work and imaging of just about every body part. The anatomy we position is the anatomy we see on the image. It’s all based on science! (Yes, anecdotes play a part.) An experienced technologist may share special tips on how to get a good odontoid image, and many times those are the things we remember. But the bottom line is that all medical imaging is based on the fundamental scientific principles of anatomy, physiology and physics. Many scientific studies validate this over and over. But... Where is the scientific evidence on mammography positioning techniques? Who made this all up? And why after all these years, do we continue to do our own thing?!
We all know that most likely, unless you have undergone standardized positioning training, most techs in your department are positioning patients differently. Think of how confusing this is for new students! Let’s say Susie, who is trained by Maggie one day, positions “her way.” Then, Susie works with Anna the next day who says, “Oh, I don’t position like Maggie. This is the way I do it.” And then on the third day with Lucinda. Susie sees that while there are similarities between positioning styles, Maggie, Anna and Lucinda are all positioning differently. Again, very confusing for a new tech!
I believe this is also one of the reasons we have such a high level of inconsistency in our images from year-to-year, and why there are so many ACR accreditation failures for poor positioning. It seems a bit wild that standardized positioning for every other body part is consistent throughout the world, but it’s not the case within our own breast imaging department for each technologist. I won’t get into how I think this happened, but I can tell you with 100% confidence that when there is a clear understanding of correlative anatomy and how it affects image quality, positioning errors are avoided and/or easily corrected. How do I know? Well, anecdotally from my 35 years of experience practicing and teaching mammography, I have seen this scenario over and over and over again. The hard part is the fact that there is not a lot of data to support me in this regard... BUT, there are a few major studies which are quite impressive and provide a clear scientific foundation for my bold statements:
All three of these studies show that the use of consistent, standardized positioning techniques improve image quality. So why aren’t we all on board? Because we missed the train in the 1990s, when positioning techniques were “perfected” and somewhat standardized, and when we had the opportunity to teach mammography technologists ‘the why’ (like we learn in general radiology), rather than just ‘the how’. Heck, at the time, I was teaching and I didn’t really understand it myself! These techniques were taught at conferences where you could learn first hand and receive actual hands-on positioning training. ASRT made the first published guidebook and ACR featured positioning in their first ACR Manual, which was published in 1994 and then updated in 1999.
Well, a lot has happened since then! We went from film-screen (FS) to Full-Field Digital Mammography (FFDM) to Digital Breast Tomosynthesis (DBT). Equipment changes necessitated that we modify positioning techniques and the 2017 AJR study² clearly showed this was possible. Unfortunately, the hands-on training opportunities diminished and positioning techniques became more diverse and inconsistent. Even companies that offer 40-hour mammography initial training courses differ greatly in how they teach positioning, adding to the confusion. But I invite you to focus on science, published studies, and information that can provide scientific evidence that those techniques improve image quality. These are your reliable sources of information.
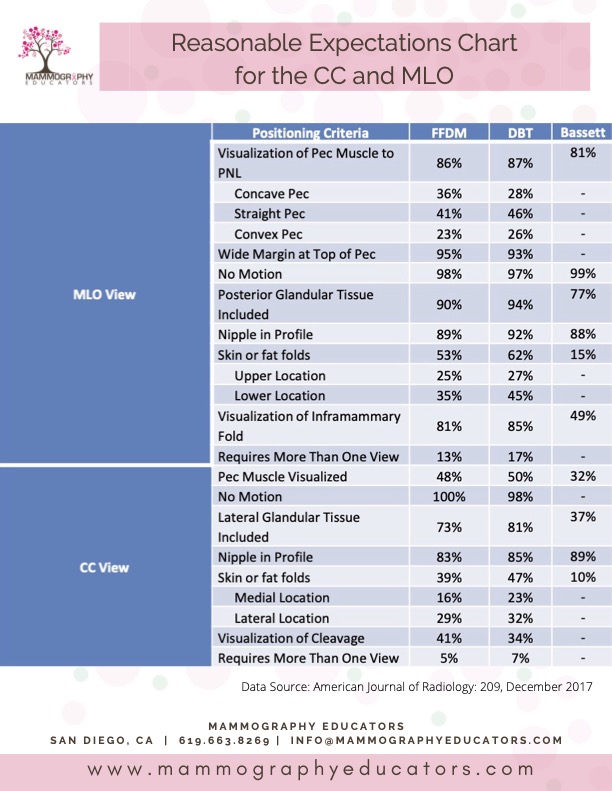
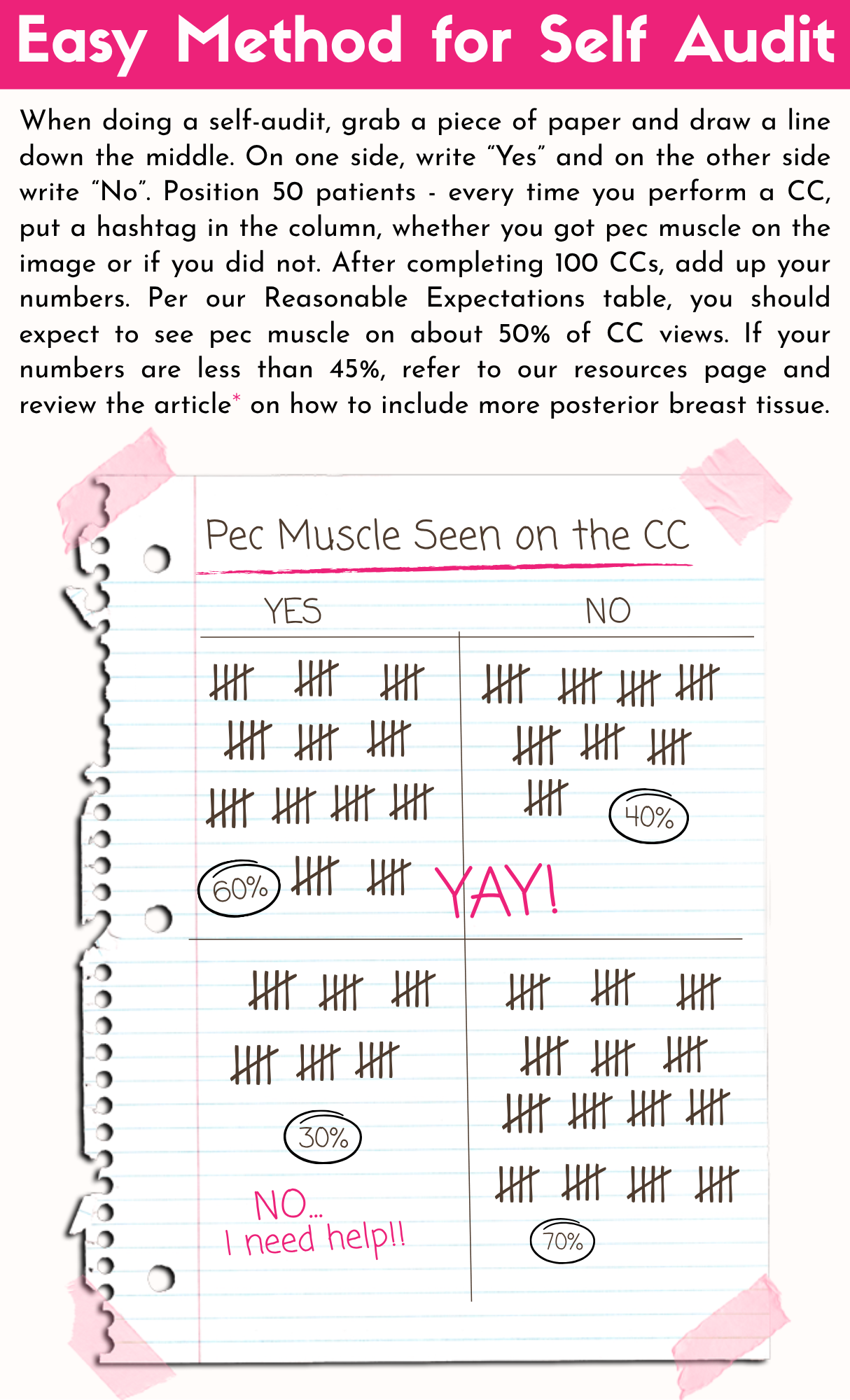
So how do you know how well you're doing compared to the expectations? If you are using standardized positioning techniques, the table below will provide you with realistic, reasonable expectations in terms of specific clinical image characteristics, and it is super easy to do a self audit!
If you are using analytical programs to evaluate your clinical images, then use that information to identify areas that need improvement. We also have many free resources on our website to help guide you!
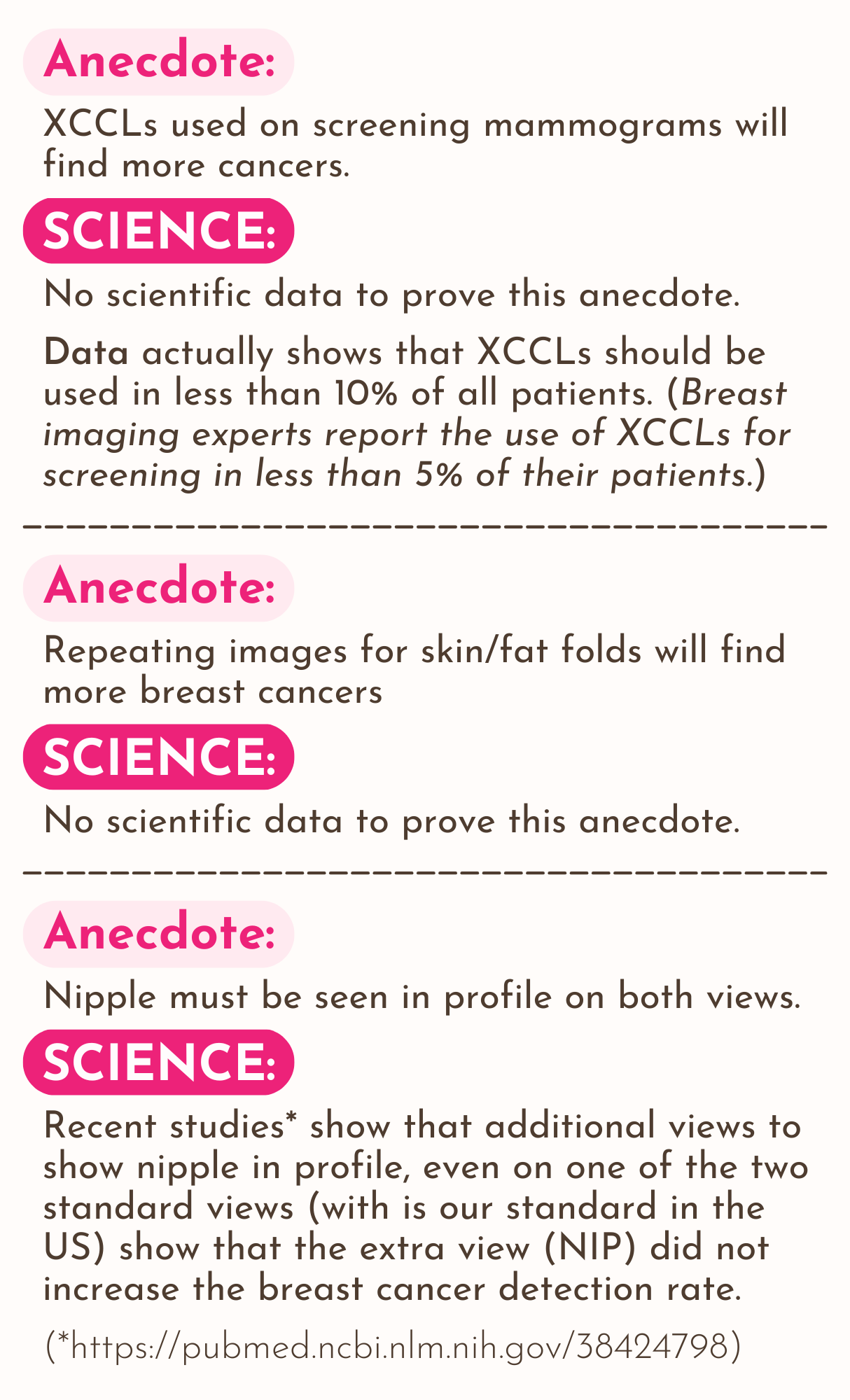
Mammography Educators wants to help you achieve the highest quality images possible that also meet scientifically proven standards and expectations, but we also understand that as techs, we all have our share of challenging patients. Remember, this is what science has proven to be true and we all know that our individual patient populations vary, so expectations may also vary. When you have a fellow tech suggest that you increase the angle for a short pec on the MLO, ask yourself, "Does that make sense?" (In my mind, no.) I strongly suggest you read articles and watch videos that will help you understand WHY you are doing what you are doing and HOW that change will make a difference in your images. It’s all science, but part of the fun of science is experimenting! I promise, if you use the positioning techniques that Mammography Educators teaches, you will be excited about the changes you see and the changes you are able to make once you have a clear understanding of the science behind it all.
References:
- Bassett LW, Hirbawi IA, DeBruhl N, Hayes MK. Mammographic positioning: evaluation from the view box. Radiology. 1993 Sep;188(3):803-6. doi: 10.1148/radiology.188.3.8351351. PMID: 8351351.
- Huppe, A. et al. (2017) Mammography positioning standards in the digital era: Is the status quo acceptable? | AJR, American Journal of RoentgenologyVolume 209, Issue 6. Available at: https://ajronline.org/doi/10.2214/AJR.16.17522 (Accessed: 25 July 2025).
- Pal, S. et al. (2018) Improving Performance of Mammographic Breast Positioning in an Academic Radiology Practice, American Journal of Roentgenology Volume 210, Issue 4. Available at: https://www.ajronline.org/doi/10.2214/AJR.17.18212 (Accessed: 25 July 2025).