Written by: Robyn Hadley, A.S., R.T.(R)(M)(ARRT), Breast Imaging Consultant
Recent headlines read: “FDA Updates Mammography Regulations in Final MQSA Rule”, “Major Updates Coming to Mammography Quality and Certification Standards….”, “FDA National Reporting Standard”, “Effective date: September 10, 2024”.
As mammography technologists and especially those of us who are responsible for regulatory compliance, we began to ask what exactly do these headlines mean? What regulations were updated? What changes does my facility have to make? Is my facility already adhering to breast density notification through my state requirements? Which regulations and requirements have the absolute and final say? Is it FDA, ACR and/or state?
I remember sitting with my inspector who would interrogate me with questions and inevitably follow up those questions with:
- "Why?"
- "Why do you do it this way or that way?"
- "Why is this quality standard measured and regulated?”
- “What is the purpose behind asking you, the facility to do this?”
- “What is the intention behind this particular FDA/MQSA requirement?”
He would truly make me think about the purpose and intention behind whatever regulation he was targeting. Many times, I wanted to answer by saying, “Well, because the FDA mandates 'it' and I have to do the task in order to remain compliant and pass your inspection!” Oftentimes, it feels like just another tedious responsibility on our to-do list.

OBJECTIVE & PURPOSE
What is new? What has changed in the FDA’s Final MQSA Rule update and why? FDA’s objective of the changes is to:
- Improve delivery of mammography services, strengthen communication
- Provide information for patients and providers to make informed decisions
- Update technological standards
- Ensure the availability of qualified personnel
- Improve mammographic interpretation through essential feedback with required metrics for the mammography medical outcomes audit analysis
A summary of the changes made by FDA are listed in three categories below. Some changes within the final rule are minor revisions pertaining to specific verbiage modifications, while others are new or specifically revised changes warranting action steps.
3 MAJOR CHANGES INCLUDE:
1) Updates that address changes in technology
2) Changes intending to enhance quality standards
3) Changes to the way mammography results are reported, categorized, retained AND transferred to patients or providers

- Facilities must retain original mammographic images and have them available for transfer upon request. (Note: FDA defines “transfer” as the conveyance of the mammogram such that the sending facility no longer retains it. For example, screen-film images are typically transferred, whereas FFDM and DBT images are usually retained in the PACS system of the sending facility and copies released upon request.)
- Facilities shall implement policies and procedures to minimize record loss. Transfer of mammograms and reports must take place within 15 calendar days of receiving the request.
- Providing timely results to patients is of utmost importance, therefore, image access and availability is essential.
- Minimizing loss of records is aimed at increasing the impact of clinical care.

- Mammograms must be submitted for interpretation in the mammographic modality in which they were originally produced and images must be retained in the original modality in which they were produced.
- To meet record retention requirements, images cannot be scanned, copied or digitized. This requirement DOES NOT apply to “comparison” images. (Note: FDA images submitted for second opinion interpretation, must be provided to the interpreting physician in their original modality.)
- The purpose for image submission in the original mammography modality is aimed to prevent possible negative implications associated with visualization of normal and abnormal breast tissue due to image quality.
- No accrediting body shall accept an application for accreditation from a facility that has failed to become accredited after 3 consecutive attempts until 1 year after the most recent failure. This will prohibit facilities from switching accrediting bodies in order to avoid the 1-year exclusion after 3 failed attempts at accreditation.
- A 1-year waiting period is believed to be an adequate time allowance for a facility to complete necessary corrective action such as mandatory training, personnel changes, etc.
- A facility’s certificate may be suspended or revoked due to a failure to comply with requests by FDA, the state certifying agency, or the AB for records/information.
- This includes clinical images for an additional mammography review (AMR) or requests for records documenting personnel qualifications.
- All devices used for mammography must be specifically designed for mammography and meet FDA approved premarket authorization requirements. Therefore, any equipment used in the acquisition, processing, interpretation, retention and retrieval of mammography images should be compatible.
- The final ruling states that “All devices used in mammography must have met the applicable FDA premarket authorization requirements for medical devices of that type and intended use”.

- Updates added the state certification agency as an entity that may initiate an AMR.
- The FDA and state certification agency can notify patients and their providers individually or through mass media when a facility is unable to perform a required PPN.
- Prior to a facility closure, the facility must arrange for access to mammography images and reports for patients and healthcare providers.
- A facility must provide personnel with copies of their MQSA qualification records.
- FDA recognizes that it is important for employees to have access to their personnel records for a period of time upon leaving a facility.
- Facilities are required to keep an employee’s personnel records for no less than 24 months from the date of the employee’s departure and be able to provide these documents to former employees for at least a 24-month time period.
- The records must also be available for review at the time of inspections occurring during that 24-month time period.
- The goal behind this requirement is to preserve access to mammography services and minimize delays in hiring new personnel.
- Upon facility closure, copies of MQSA qualification records must be provided to personnel.

- Mammographic reports must include facility name and location to include, at a minimum, city, state, zip code, and telephone number. Facilities may choose to add additional information such as an email address, records storage site, or additional information about the healthcare network/organization.
- Results letters must be provided to patients within 30 days of the examination date. The letters must include, at a minimum, name of the patient, name, address and telephone number of the performing facility, and a breast density assessment as described below.
- The final rule updated the explanatory language in the “Benign” final assessment category and added three new categories of assessment to the existing categories in regulation.
- The two “Incomplete” assessment categories are taken from the 2003 approved alternative standard #11: “Incomplete: Need additional imaging evaluation” and “Incomplete: Need prior mammograms for comparison”.
- The incomplete categories must be utilized individually as each has different reporting requirements.
- Assessment category “Incomplete: Need prior mammograms for comparison” requires that a follow-up report be issued within 30 calendar days of the initial report whether or not comparison views are obtained.
- Assessment category “Incomplete: Need additional imaging evaluation” does not have a specified time frame requirement for a follow-up report.
- “Post-Procedure Mammogram for Marker Placement” is almost identical to the 2003 approved alternative standard #12. This category also helps facilities identify and exclude this assessment category from the medical outcomes audit data.
- For mammogram reports with the final assessment of “Suspicious” or “Highly Suggestive of Malignancy”, the report to the provider and result lay letter to the patient must be sent within 7 days of the final interpretation of the mammogram.
- The time-frame for sending all mammographic reports and results lay letters is 30 days from the date of the examination.
- All facilities must use a national dense breast reporting standard for all patients for both mammogram reports to healthcare providers and result lay letters to patients.
- Both reporting standards state the tissue density and recommend the patient talk to their provider about breast density and their individual situation. At a minimum, the standardized language stated below must be included and cannot be altered. (Refer to "Not Dense" and "Dense" outlined below.)
- Facilities may choose to add additional information.
- Most importantly, for facilities in states that already require specific density notification, this information can be included, but must be distinctly separate from the FDA required language. (NOTE: Facilities need to comply with all federal, state and local requirements.)
- With breast density notification, the FDA estimates a reduction in mortality and reduced cost of breast cancer treatments.
- The intention of the final rule is to provide information to patients and providers to help guide care.
- The goal is also to ensure that patients are given a consistent baseline of information regarding their breast density.
- “Breast tissue can be either dense or not dense. Dense tissue makes it harder to find breast cancer on a mammogram and also raises the risk of developing breast cancer. Your breast tissue is not dense. Talk to your provider about breast density, risks for breast cancer, and your individual situation.”
- “Breast tissue can be either dense or not dense. Dense tissue makes it harder to find breast cancer on a mammogram and also raises the risk of developing breast cancer. Your breast tissue is dense. In some people with dense tissue, other imaging tests in addition to a mammogram may help find cancers. Talk to your provider about breast density, risks for breast cancer, and your individual situation.”
- The mammography medical outcomes audit report must contain specific information collected and calculated by facilities. At a minimum, the metrics required to be reported on include positive predictive value (PPV), cancer detection rate (CDR) and recall rate (RR).
- Tracking specific metrics is essential in evaluating the accuracy of detecting breast cancer and identifying areas of opportunity for improvement.
DESIGN
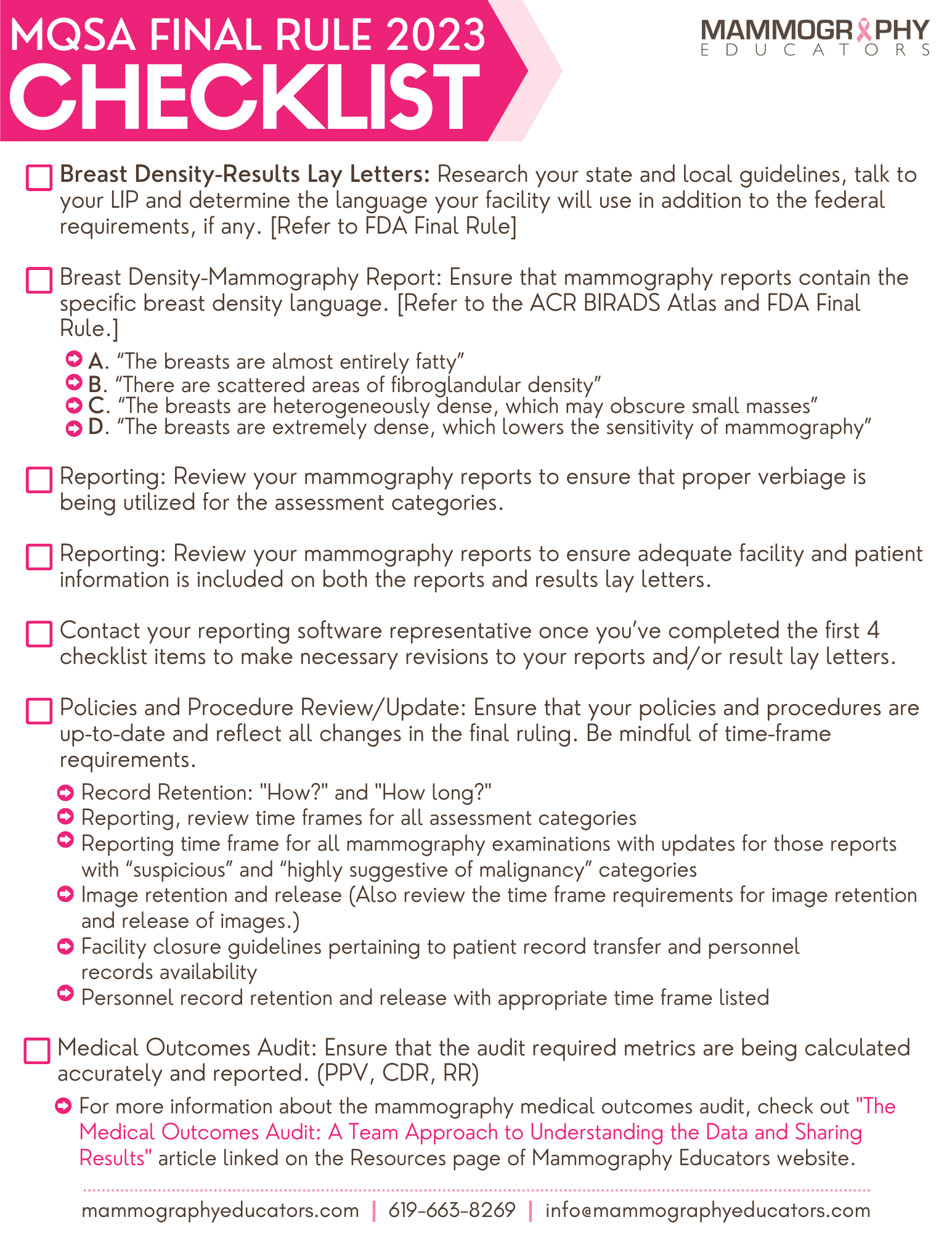
Now that we have a general idea of the final rule updates to the FDA mammography regulations, we can turn attention to the “DESIGN” of our programs with compliance and best practice in mind. "But, where do we begin?" I am so glad you asked! Who else appreciates a good checklist? I LOVE checklists! The following is a checklist of items to get you started. Begin using this checklist to review and update your policies, procedures and general practices to ensure you are compliant by September 10, 2024. This can also be a great resource to use for discussions with your radiologist(s) regarding adhering to and complying with regulations, but also exploring new ideas for implementing best practices within your departments.
Bottom line:
Regulatory compliance may be the responsibility of one or two designated individuals within your organization, but it is the responsibility of ALL team members to uphold the rulings. Doing so is essential to keeping best practice design at the core of what your team does. In the midst of these changes, it is imperative to remember that caring for our patients and protecting their precious moments of life is the “why” that drives the design.
REFERENCES:
- Federal Register. https://www.federalregister.gov/documents/2023/03/10/2023-04550/mammography-quality-standards-act#print. Accessed March 2023
- Densebreast-info. https://densebreast-info.org/. Accessed March 2023
- Berg, W., Seitzman, R., Pushkin, J., Implementing the national dense breast reporting standard, expanding supplemental screening using current guidelines, and the proposed find it early act. Journal of Breast Imaging, 2023. wbad034. Retrieved April 2023, https://doi/org/10/1093/jbi/wbad034
- Jacobs S, Hadley R. The medical outcomes audit: a team approach to understanding the data and sharing results. SBI News Spring 2022. Society of Breast Imaging. Published on March 1, 2022. https://mammographyeducation.com/the-medical-outcomes-audit-a-team-approach-to-understanding-the-data-and-sharing-results-sbi/



