Repeats, Rejects and Recalls:
How Many is Too Many?
By Louise C. Miller, ARRT, CRT, RTRM
The Member Newsletter of The Society of Breast Imaging, 2015, Issue 2, pages 5-6
Recently, I was asked to work in a breast imaging facility and conduct an on-site positioning workshop. The radiologist said that the facility had high level of "TCBs," and he worried about the increased, unnecessary additional radiation a dose to the patients. I was embarrassed as I had never heard that acronym used and was not sure what it stood for. It meant: Technical Call Backs.
Our Audience Often Asks:
Ahh…no wonder... we rarely have TCBs. I spent a week at the facility. A year later, he emailed me and said that they had reduced TCBs by 50%! Unfortunately, the data were not published.
I was surprised when several technologists at another breast center informed me that exaggerated craniocaudal to the lateral (XCCL) views were performed on approximately one third of their patients. Their radiologist wanted them. This was not just at one site, but at many: too many extra views on patients who did not require them. The standard screening mammogram had become a six or eight view exam. This was odd as all repeat/reject rates were well within compliance at these facilities.
Many technologists are told that they MUST repeat every image that does not show the inframammary fold (IMF) or those that show skin/fat folds. So they obtain the repeat images and are still in "compliance." Technologists have many options to choose from when stating the "cause" of the repeat/reject; one can unknowingly skew the statistics based on several options selected prior to the exam being performed. The technologists are also unnecessarily exposing the patients to additional radiation and anxiety.
Unfortunately, very little data have been published on these issues. One of the last studies predates the implementation of full field digital mammography (FFDM) and digital breast tomosynthesis (DBT). In 1993, Bassett et al. evaluated 2000 film-screen (FS) mammograms and created a standard for excellence in image quality (1). Interestingly, none of the criteria were met 100% of the time. However, after the technologist received "standardized" positioning training, image quality improved by 68% (1). Still, overall image quality standards were met only 64% of the time (1).
Currently, there seems to be an expectation from many radiologists that all images should be of American College of Radiology (ACR) quality every time, which is quite an unreal expectation, given that most of us search for weeks to find the "perfect" fatty and dense breasts to submit for accreditation.
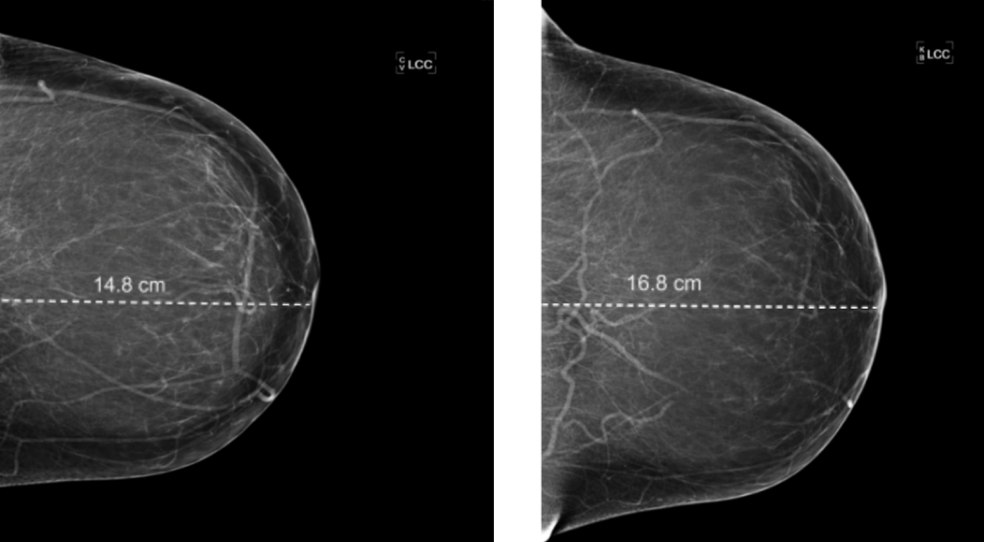
There have been marked changes and technologies since the study by Bassett et al. was published (1). Image receptors and face shields have increased in size. The imaging format is completely different. These factors often provide a challenge for technologists and radiologists.