Written by: Robyn Hadley, A.S., R.T.(R)(M)(ARRT)
My radiologist is reading off-site now! What are the regulations and requirements to remain compliant? How do I acquire all the necessary information? How can I make sure I have and maintain documentation to satisfy my inspector? The use of telemammography has the potential to improve healthcare delivery and access by uniting patients with breast specialists (Chung and Parikh, 2020). Balancing patient accessibility and quality patient care requires us to be diligent in a number of factors when considering and implementing telemammography into our practices. Check out these tips, FAQ’s and final checklist to help regulate, not complicate!
Quality Control and Regulatory Requirements
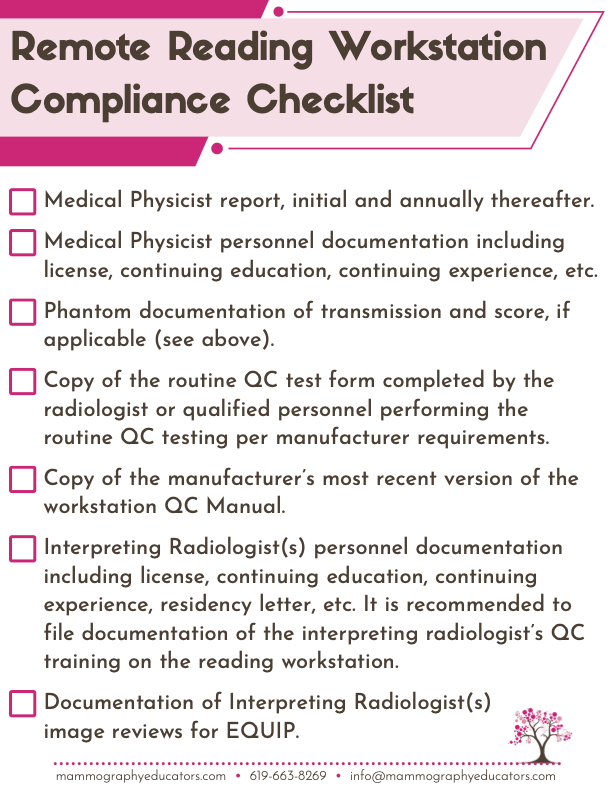
For facilities utilizing telemammography services with offsite radiologist reading workstations, Warren Freier, MQSA Inspector, offers the following guidance: the “facility must provide the same documentation for off-site workstations as is required for on-site, in house workstations. This information should include personnel qualifications, QA, QC, program review, etc.” Operational components of telemammography include image transmission, storage, display and reporting.
1) Image Transmission and Storage:
- Facilities must ensure there is adequate means to securely and confidentially exchange data with appropriate transmission speed.
2) Display Monitors/Radiologist Reading Workstation:
- Meet minimum resolution and luminance requirements for mammography interpretation
- Medical Physicist (MP) Testing:
- For newly installed workstations, the medical physicist must test the workstation prior to mammography interpretation.
- For existing workstations (i.e.: your facility is joining a telemammography group), the workstation must have documentation of MP testing within the previous 14 months.
- Note: Tests that evaluate the performance of the entire imaging chain, such as the phantom and other tests listed in the FFDM manufacturer’s or accessory component’s QC manual, require the MP to perform tests on those accessory components prior to use in patient examinations. Prior tests cannot be used in this instance (FDA).
3) Quality Control Test:
- Ensure that weekly quality control tests are completed by the qualified off-site staff/radiologist per the manufacturer or ACR DM QC manual. The facility who holds the MQSA certificate is the entity that is ultimately responsible for ensuring that routine tests are completed and appropriate documentation is obtained.
- Facilities joining a reading group should make arrangements to ensure this is carried out routinely by qualified individuals and documentation of such tests is made available.
- Facilities who transition to an in-house radiologist reading remotely must ensure that the radiologist is properly trained to carry out QC testing and is performing the routine QC testing. Documentation of testing should be made readily available.
- Many manufacturers have the capability to set the routine testing to run on a specific date/time automatically. In any case, the technologist must log in to retrieve documentation and verify that the test results are within acceptable limits. If login is not available, uploading or entering test data to a shared drive/folder is an effective way to make the information readily available to all necessary staff.
Tips For a Successful Team Approach
Communication and standardized practices are key to implementing and maintaining a successful telemammography relationship. Upon implementing a remote reading/telemammography practice, clear expectations about the established processes, procedures, practices and personnel should be effectively communicated. Designating qualified personnel to ensure that quality imaging is maintained and all quality assurance practices remain compliant is crucial. Qualified personnel must be adequately trained and educated on QC procedures, and stay up to date on regulations, requirements and manufacturer upgrades. Utilizing resources such as shared files and/or software programs with current, regularly updated QC data that can be easily accessed at any time by all applicable individuals can be helpful and time-saving.
Although telemammography services are on the rise, up 22% from 2019-2022 (VRAD), access to services and fellowship trained breast imaging specialists, which make up only 10% of all radiologists (Lewis et al., 2006), is challenging in the current healthcare setting. With subspecialist radiologists being few and far between, there are not enough to go around. Sickles et. al. reported that breast specialists detect more cancers overall with higher screening cancer detection rates and lower recall rates. Breast Specialists report a cancer detection rate of 6.0 versus 3.4 per 1000 screening exams and a recall rate of 4.9% versus 7.1% compared to general radiologists (Sickles et al., 2002 & 2005). Additionally, in counties with inadequate availability of mammography machines, there is a 13-15% reduction in screening compliance (Elkin, 2010).
Telemammography continues to play an important role in breast health accessibility, therefore it is equally as important to be attentive about quality requirements for image viewing and interpretation.
Frequently Asked Questions:
Medical Physicist survey, personnel documents for the MP and interpreting radiologists, weekly/annual QC tests, documentation of service and/or upgrades to the workstation
It is not required. Refer to manufacturer specific guidelines. Documentation in the QC file should reflect notes indicating there were no mammography examinations interpreted during that time. QC testing may be required prior to interpreting mammography examinations upon the radiologists return to work.
It is not required to send the phantom to the reading workstation routinely. However, if the remote reading workstation and/or telemammography group is new to your facility, you may have to send a phantom to the reading workstation to verify appropriate image transmission and performance of the entire imaging chain.
Yes. If the Medical Physicist is different from the MP at your facility, you must also keep that MP’s personnel documentation on file.
Yes. All Radiologist Workstations that are used to interpret mammography images for facilities using the ACR DM QC manual must also implement the ACR DM QC manual for all applicable Radiologist Workstations.
Yes. The location and/or name of the workstation should be clearly identified on the QC reporting form.
You will need the same documentation required as an on-site reading workstation such as personnel documents for the interpreting radiologists and medical physicist, annual MP survey, routine QC reports, EQUIP reports for the interpreting radiologists, etc.
Yes. Your medical physicist and/or manufacturer should be able to provide you with this information.
References:
- Chung, Hannah and Parikh, Jay, Telemammography: Technical Advances Improve Patient Access in Breast Care, Journal of Breast Imaging, Volume 2, Issue 2, March/April 2020, Pages 152–156, https://doi.org/10.1093/jbi/wbz088
- Elkin EB, Ishill NM, Snow JG, et al. Geographic access and the use of screening mammography. Med Care 2010; 48: 349–356.
- Lewis RS, Sunshine JH, Bhargavan M. A portrait of breast imaging specialists and of the interpretation of mammography in the United States. AJR Am J Roentgenol 2006;187:W456–W468.
- Policy Guidance Help System. FDA. Accessed on August 7, 2024 at: https://www.accessdata.fda.gov/cdrh_docs/presentations/pghs/PGHS_Main.htm
- Sickles EA, Miglioretti DL, Ballard-Barbash R, et al. Performance benchmarks for diagnostic mammography. Radiology 2005;235:775–790.
- Sickles EA, Wolverton DE, Dee KE. Performance parameters for screening and diagnostic mammography: specialist and general radiologists. Radiology 2002;224:861–869.
- The American College of Radiology Digital Mammography QC Manual: Frequently Asked Questions. 2024. Accessed on August 7, 2024 at: https://www.acraccreditation.org/-/media/ACRAccreditation/Documents/Resources/DMQC/DMQCFAQs.pdf