Written by: Louise Miller, R.T.(R)(M)(ARRT), CRT(M), FSBI, FNCBC and Erin Ferraro, M.S., R.T.(R)(M)(ARRT)
Repeats and rejects are one of the most misunderstood and misused aspects of all mammography quality assurance processes. When should you repeat an image and when should you reject it? You think to yourself, "We got IMF last year, but I don't have it this year. Let’s blame it on the patient... Reject. Positioning challenges... Repeat. Body habitus... Not my fault. But should I still send them all through? Do I want that 'crummy' image without IMF, even when I can see it on the second round of images? Rad A wants to see them ALL, but Rad B only wants to see four ACR perfect images."
See? It's NOT easy! The Repeat/Reject Analysis is a test required by MQSA that has to be performed quarterly. The goal of this test is to assure the quality of our mammograms. By tracking the repeat and reject rates, we can identify and address specific issues that may lead to poor image quality due to positioning problems and/or equipment problems. This data allows for identifying areas for improvements in technologist training, machine calibrations, and imaging protocols, ultimately enhancing overall image quality and patient experience. So, let's get started with some definitions (1).
- What: An analysis of repeated/rejected clinical images must be performed, analyzed and documented.
- Rates: Not to exceed greater than 5% of total images. *Average rate: 2.62% (2)
- Calculations:
- Reject Rate = The number of rejected images divided by the number of examinations
- Repeat Rate = The number of repeated images divided by the number of examinations
- Frequency: Calculated quarterly
- Operating Level: Less than 2% change up or down from previous rate
The Exception: You may have an experienced technologist who practices standardized positioning techniques and their repeat/reject rate is normally within limits, but if you are training a new technologist, have students on-site or equipment updates, those numbers will change, and that’s okay. In fact, it is expected during training. However, that rate should return to acceptable limits within a reasonable period of time.
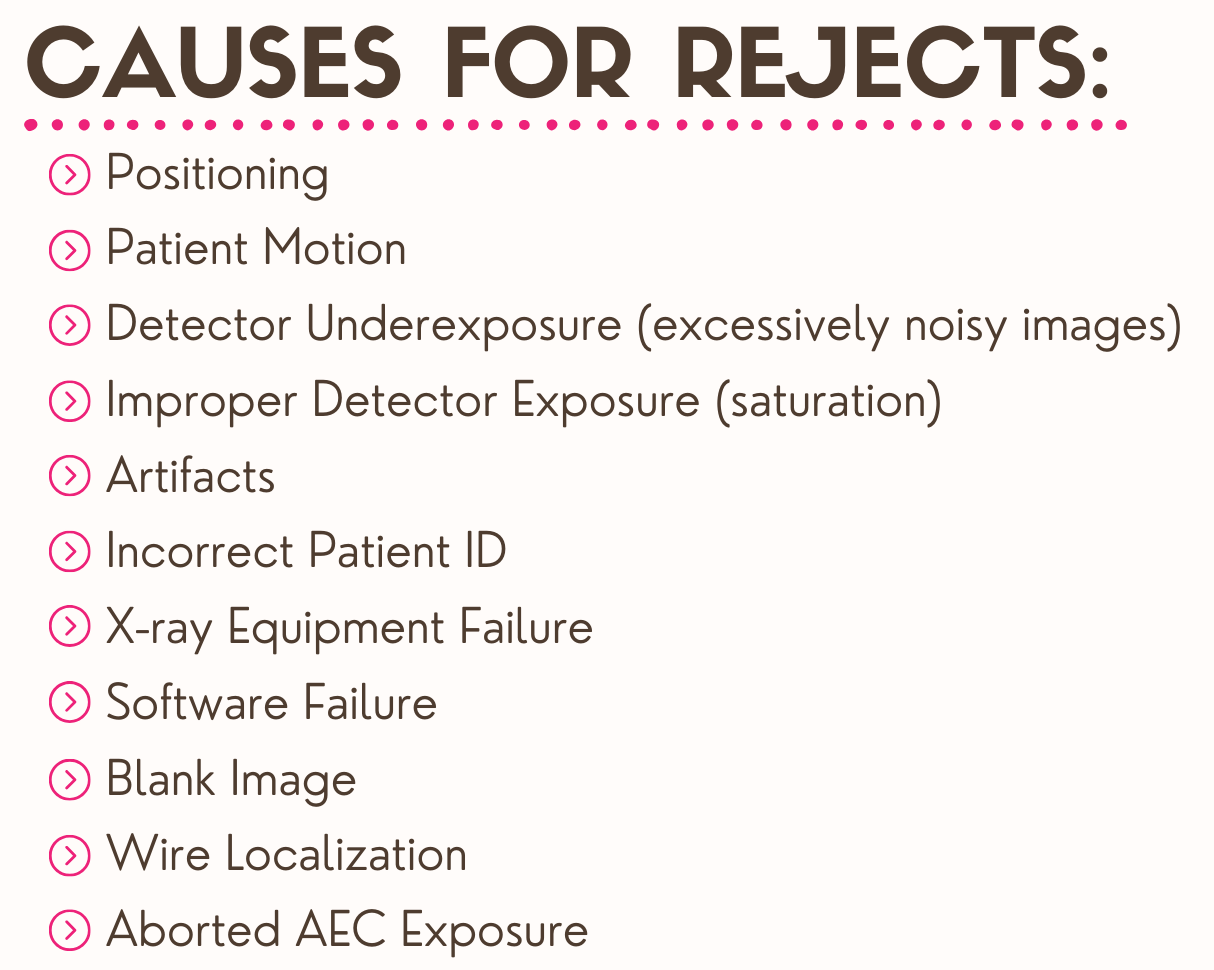
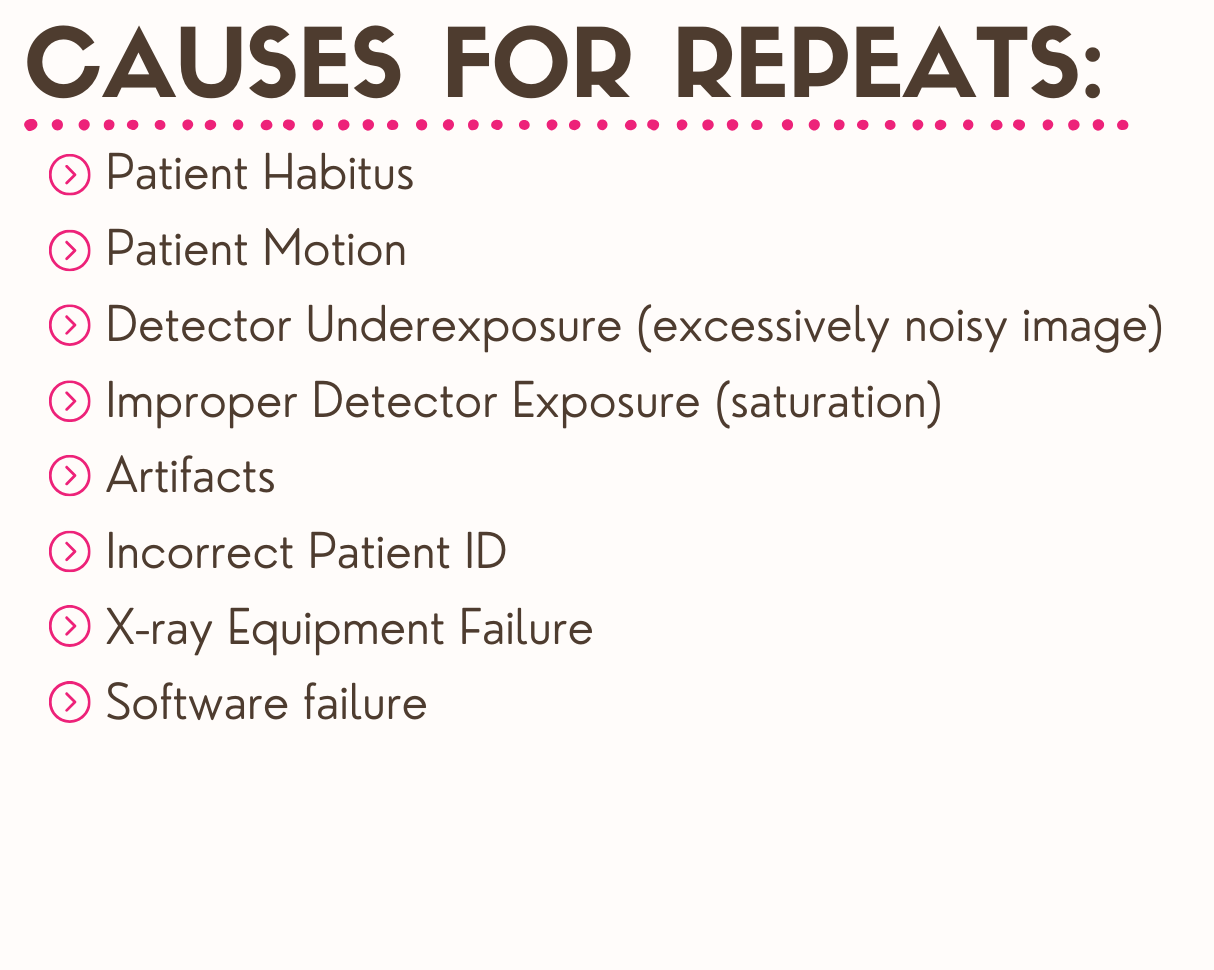
It's important to select the proper reason for your repeat/reject image:
Examples of positioning reasons include:
- Exclusion of breast tissue (not related to breast size)
- Breast excessively drooping on MLO (not related to breast size)
- PNL on the CC view inadequate compared to the MLO view
- Inadequate pectoralis muscle on the MLO view.
Examples of body habitus reasons include:
- Large breasts that need to be tiled/mosaicked
- Patients with limited range of motion
- Patients with skeletal deformities, such as pectus carinatum/excavatum, etc.
TIP: How do you know if it is a positioning error or the patient's body habitus? Remember the mantra: "Meet, Beat, Repeat". Look at patient's previous images and determine if the tech was able able to achieve acceptable image quality? If you did not "meet" or "beat" those images, then it is most likely a positioning error and you should repeat the image. However, if the patient has experienced physical changes since their last mammogram (e.g., shoulder surgery, excessive amount of weight loss, etc), then the correct reason for the repeat would be body habitus.

Do NOT stop exposures (mid-exposure) when you see the preview/raw image and determine that the positioning is substandard.
This is referred to as “aborting” the exposure and may (depending on the machine manufacturer) result in a message such as “exposure released prematurely.” It has been reported that some technologists do this so the “aborted” exposure will not count towards their repeat/reject rate. However, I would strongly advise against this, as it is not only unethical, but also illegal to falsify reported data (even if unintentional) that is required and mandated by federal law (MQSA). Also, it will not provide accurate dose information for the patient. This practice is strongly discouraged.
Do NOT call it something that it is not.
If you have excluded breast tissue, check positioning. "Other” should not be your default to justify poor images resulting from the use of poor positioning techniques. We want to identify ongoing problems so we can learn from them and find solutions to help improve!
A few years ago I wrote an article for the SBI Newsletter called, Repeats, Rejects and Recalls: How Many is Too Many? It contains information you may find helpful, including a section related to Common Causes and Solutions for Repeat and Reject Images and Unnecessary Additional Views. Some additional recommendations when it comes to repeats and rejects include:
- Developing policies and procedures related to repeats/rejects and the use of proper documentation.
- Making sure staff consistently follows facility guidelines.
- Look for downward trends and address issues through individual coaching, appropriate resources and encouragement. (Technologists want to do better!)
- Look for upward trends and provide positive feedback to individuals and staff. (They also want to know when they are doing well!)
Additionally, artificial intelligence (AI) is becoming increasingly popular within healthcare and mammography specifically. It can be very helpful in managing repeat/reject rates. AI helps mammographers by providing real-time feedback on image quality and positioning during the patient’s exam. It can also assist in identifying potential issues such as inadequate compression or patient positioning. This allows the technologist to make immediate adjustments, therefore reducing the probability of rejected images and the need for repeated screenings/technical call backs. Although there may be a learning curve when beginning to use AI, ultimately it will lead to empowering technologists and ensuring the highest quality images are being acquired.
Bottom Line: In order to use the repeat/reject analysis properly and effectively it is imperative to be honest and use the objective data to celebrate your excellence or identify opportunities for improvement.
REFERENCES:
- Mammography Quality Standards Act, 2002. Accessed on February 6, 2024 at: https://www.fda.gov/radiation-emitting-products/regulations-mqsa/mammography-quality-standards-act-regulations
- Mercieca, N., Portelli, J. L., & Jadva-Patel, H. (2017). Mammographic image reject rate analysis and cause - A National Maltese Study. Radiography (London, England : 1995), 23(1), 25–31. https://doi.org/10.1016/j.radi.2016.07.004