Written by: Louise C. Miller, R.T.(R)(M)(ARRT), CRT(M), FSBI, FNCBC, Director of Education
There is so much discussion regarding visualization of the Inframammary Fold (IMF) on the Quality Breast Imagers (QBI) Facebook Page, I thought it would be appropriate to write a blog and share my thoughts about recommendations that have been made.
Let’s start with some info on the IMF:
- IMF is the inferior border of the breast and the crease between the breast and abdominal tissue. On the MLO, it is important to include some abdominal tissue to visualize the IMF in the open position.
- IMF serves as an important anatomical landmark on an MLO to provide assurance to the technologist and radiologist that all of the inferior, posterior breast tissue has been included.
- Data shows that after updated, standardized positioning training for digital platforms, the IMF can be visualized as follows: FFDM 81% and with DBT 85% of the time. (AJR:209, December 2017)
- Folds in the IMF are visualized as follows: FFDM 35% and with DBT 45% of the time. (AJR:209, December 2017)
What defines the visualization of the IMF??
There is no published data regarding the definition of the visualization of the IMF, including the 1999 ACR Manual. How much is enough? Is just a “sliver” OK? Is 2-3 cm too much? Here are the definitions I have come up with… and again, these are just my definitions. As I am not an ACR reviewer, and cannot find any published definition for a description of the IMF, the basis for this information is from my teachings from several preeminent radiologists that I have had the opportunity to work with. Your radiologist may feel differently, but based on my opinion and experience, this is how best I define the visualization of the IMF:
- IMF is “visualized” when you see a downward turn from the breast to the abdomen, no matter how slight.
- The IMF is considered “open” when there are no folds seen vertically or horizontally.
- Folds in the IMF are common and normally do not impede diagnosis. Here’s the data: Folds are seen in the IMF on 35% of all images done with FFDM and 45% with DBT. (AJR:209, December 2017)
As the radiologist can scroll through skin and fat folds images, I believe that the study should not be repeated if the folds do not impede diagnosis by examining this area with DBT. Most skin and fat folds are radiolucent and thus will not hide any area of concern. Therefore, I would not repeat images if the folds can be visualized with the use of DBT. It is not necessary and will result in unnecessary exposure to the patient.
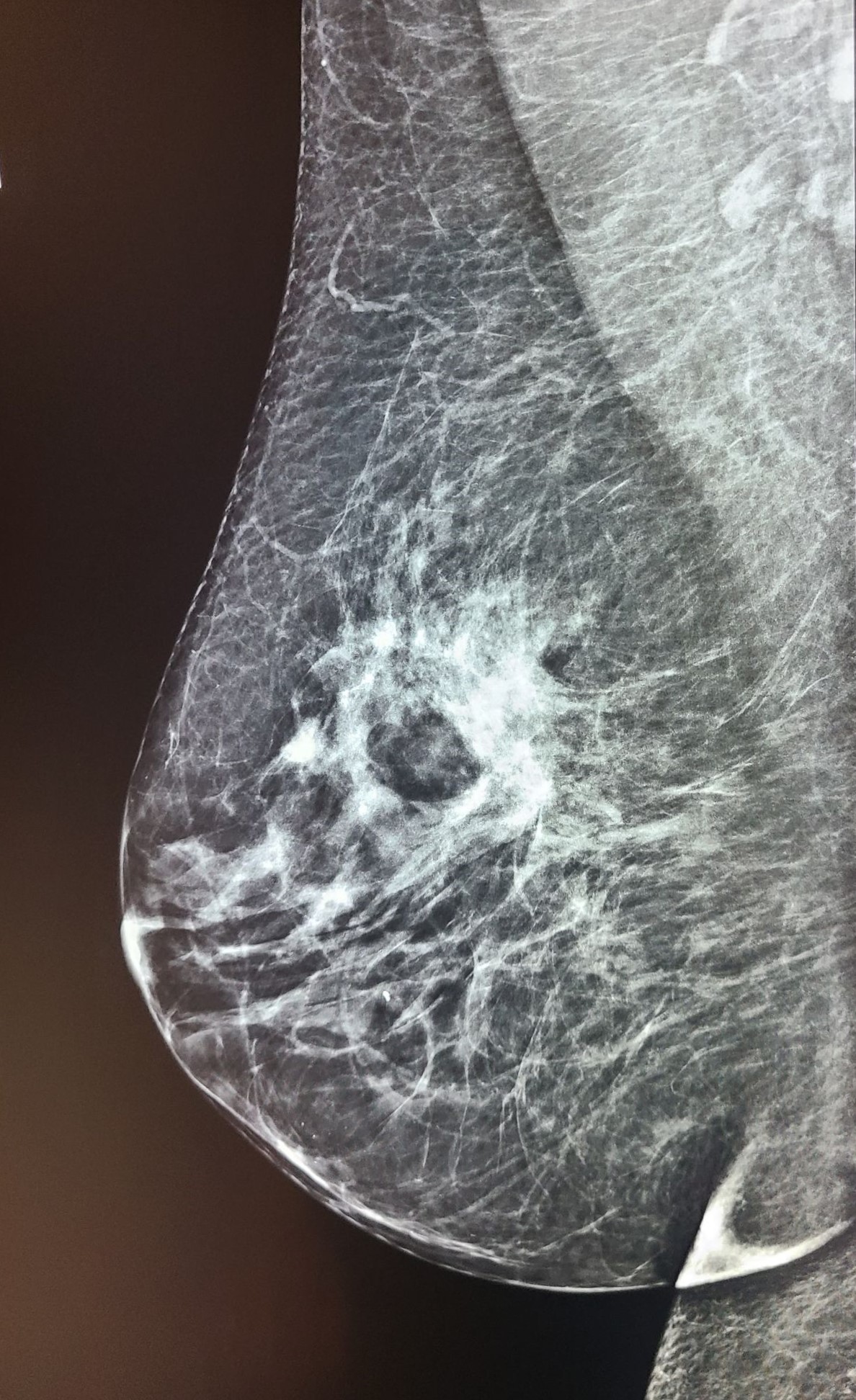
Obviously I cannot make assumptions about what is acceptable to your individual radiologist, but this is my professional opinion. I can tell you that many mammo techs have sent me images of MLOs with folds and asked if they felt it was a “repeatable offense” (See Figures 1, 2, 3 below).

Figure 1 (Click to view full size image)
Figure 2 (Click to view full size image)
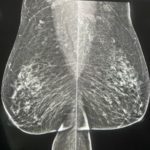
Figure 3 (Click to view full size image)
I have sent these images to some of the most experienced radiologists in the country who are highly respected. They unanimously replied saying, “No, they would not repeat.” Perhaps this will help facilitate a conversation with your radiologist so that you will understand their position on this issue.
Bottom line: It might not look ACR perfect (and thus not be a good candidate for Accreditation) or “pretty”, but I am referring to what we see on the average screening patient. If the image is of diagnostic quality, I would not repeat it.
It is important to understand that it is IMPOSSIBLE to visualize IMF on every patient.
As I previously wrote in the SBI Newsletter: “Please note that regardless of the experience and expertise of the technologist, the “perfect” image cannot be produced 100% of the time.” In fact, in one study (Bassett et al., 1993), it was shown that only 67% of mammograms met the “criteria”of a good mammogram. This was due to variations in body habitus and other patient circumstances. The same study, done on film screen images, showed visualization only 47% of the time!
Recent published data (AJR:209, December 2017) shows that after proper training for FFDM and DBT, this number increased markedly. While this is significantly better, especially given the increased width, length and thickness of the IR, this data confirms that we cannot visualize the IMF on every patient. So how do you know when you can or cannot expect to see the IMF? A good way to judge if this is possible is to look at the previous images. If the previous images had IMF and there has been no significant change in patient body habitus or patient mobility/flexibility since their last exam, you should be able to visualize IMF on this exam. If many previous studies show that IMF was not included, of course I would try to include it on this year’s images, but I would not recommend taking multiple, repeat images to try to accomplish this.
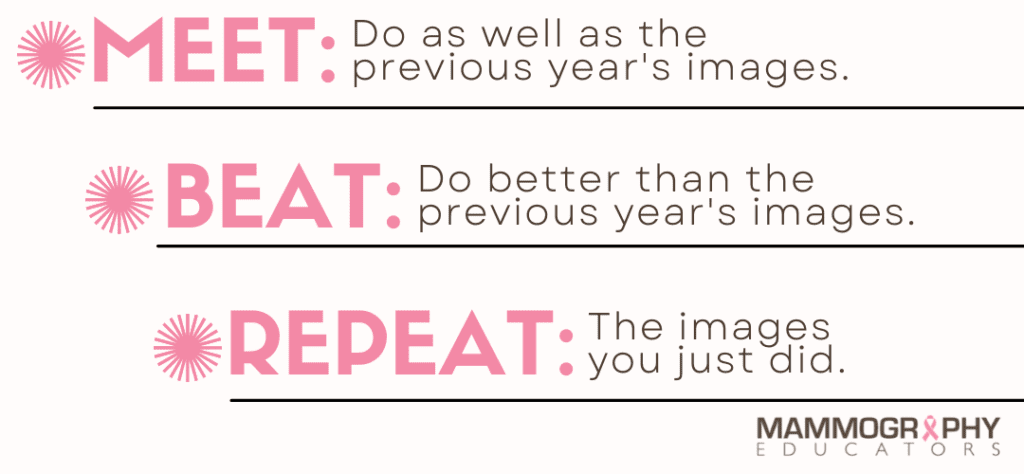
Years ago a radiologist friend of mine, Dr. Jay Parikh from MD Anderson Cancer Center in Houston TX (who is a great supporter and educator of mammography technologists!) taught me a great phrase and rule of thumb that I still try to follow:
Recently I have been thinking that there is most likely a relationship between visualization of IMF (and CV) and body mass index (BMI), breast size and density. But as I said previously, the only published data suggests that it can be visualized about 85% of the time. Why is it important to know that number? Because if you are not at least within 10% of the benchmark, it tells you very specifically that every effort should be made to learn new techniques that will get you close to this number. So how do you know how often you are getting IMF?
Do a self audit. Here’s how:
- If you use Volpara Enterprise or another A.I. program you can access this data easily.
- You can do a manual count. Grab a blank piece of paper and draw a vertical line down the middle. On one side write “Y” and on the other side write “N”. For every MLO that you do, indicate with a hash mark on your paper whether or not the IMF is visualized: “Y” for Yes or “N” for No. The IMF does not need to be perfect! (See notes below.)
- You should do about 200 MLOs (that’s just 100 patients, with maybe a few unis thrown in). Then add up the hash marks. You should have about 140 in the “Yes” column which gives you 70%!
So what if your number is below 70%?
What can you do? Here are things you should consider:
- Tube angle does not usually affect visualization of the IMF, BUT a too steep angle (over 50 degrees) will decrease the chances of including it.
- Visualization of the IMF is almost always due to the patient's position!
Patient Position
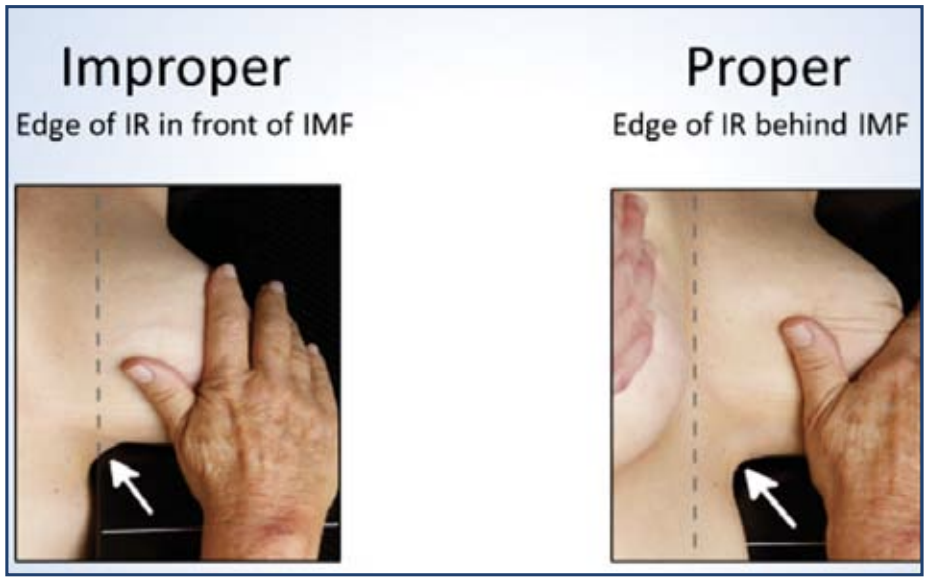
The position of the patient relative to the bottom front corner of the IR is critical (Figure 4):
- The patient must be facing forward, towards the mammography machine.
- The lower front corner of the IR should be directly below the patient’s nipple and halfway between her anterior-superior iliac spine (ASIS) and umbilicus.
- This positioning requires the patient to step towards the technologist, who should be standing at the medial side of the breast to be imaged.
- I do not have the patient bend at the waist or abduct her hips (push her butt out). This pulls the IMF out of the field of view.
- I do not do a “two finger sweep” unless there are prominent folds that can be eliminated.
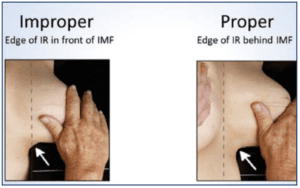
Figure 4. Proper positioning is achieved by lifting the breast and bringing the IMF (arrow) onto the image receptor. The dashed line indicates the edge of the IR.
FINAL BEST TIP EVER!
One day I was positioning a MLO on a patient with large, heavy breasts. I asked her to flatten her other breast as it was in the way of the path of the compression paddle. (NOTE: I never would ask the patient to pull her breast back because then she will end up pulling the breast I am imaging along with it! This would mean I would lose valuable visualization of medial breast tissue.)
Anyway, she flattened her breast and lifted it up. Not sure why, but when I was looking at her IMF while she was lifting her breast it was like the folds all but disappeared. It was almost a miracle! I could not believe my eyes!! So while I wish I could claim this idea was mine and thus name it the “Miller Miracle Maneuver,” I am just the recipient of some very good luck and can now pass the “Miracle” on to you. (See Figure 5.) Try it. You'll like it!
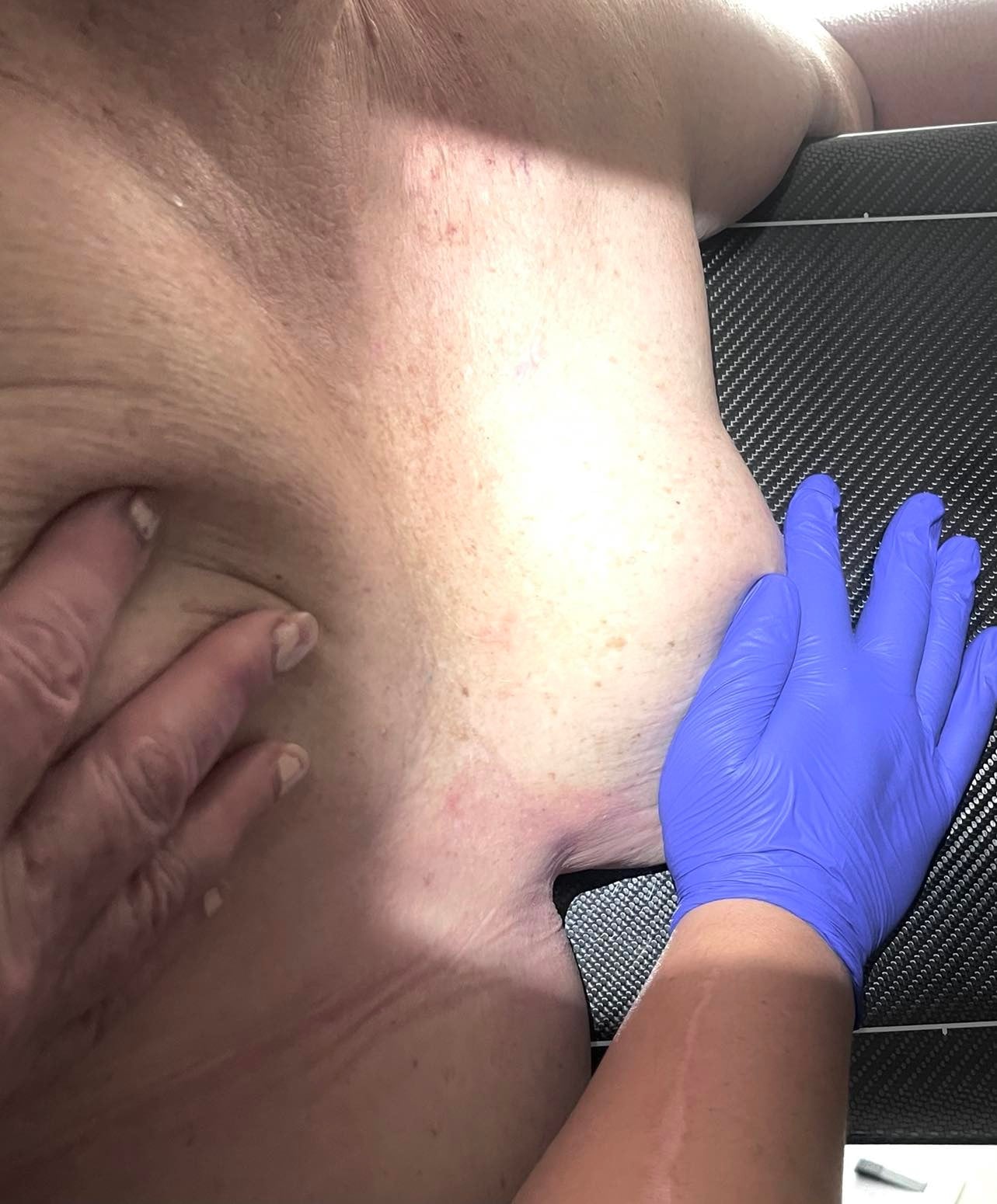
Figure 5 (Click to view full size image)
While I hope these suggestions are helpful, remember... There is no “magic bullet”. Do the best you can given this new information and let me know how it goes!
References:
Bassett LW, Hirbawi IA, DeBruhl, N, Hayes MK. Mammographic positioning: evaluation from the view box. Radiology. 1993;188(3):803-806)
Huppe A., Overman K., Gatewood J., Miller L., Inciardi M., Mammography Positioning Standards in the Digital Era: Is the Status Quo Acceptable? American Journal of Roentgenology (AJR) 2017.