Written by: Louise C. Miller, R.T.(R)(M)(ARRT), CRT(M), FSBI, FNCBC, Director of Education
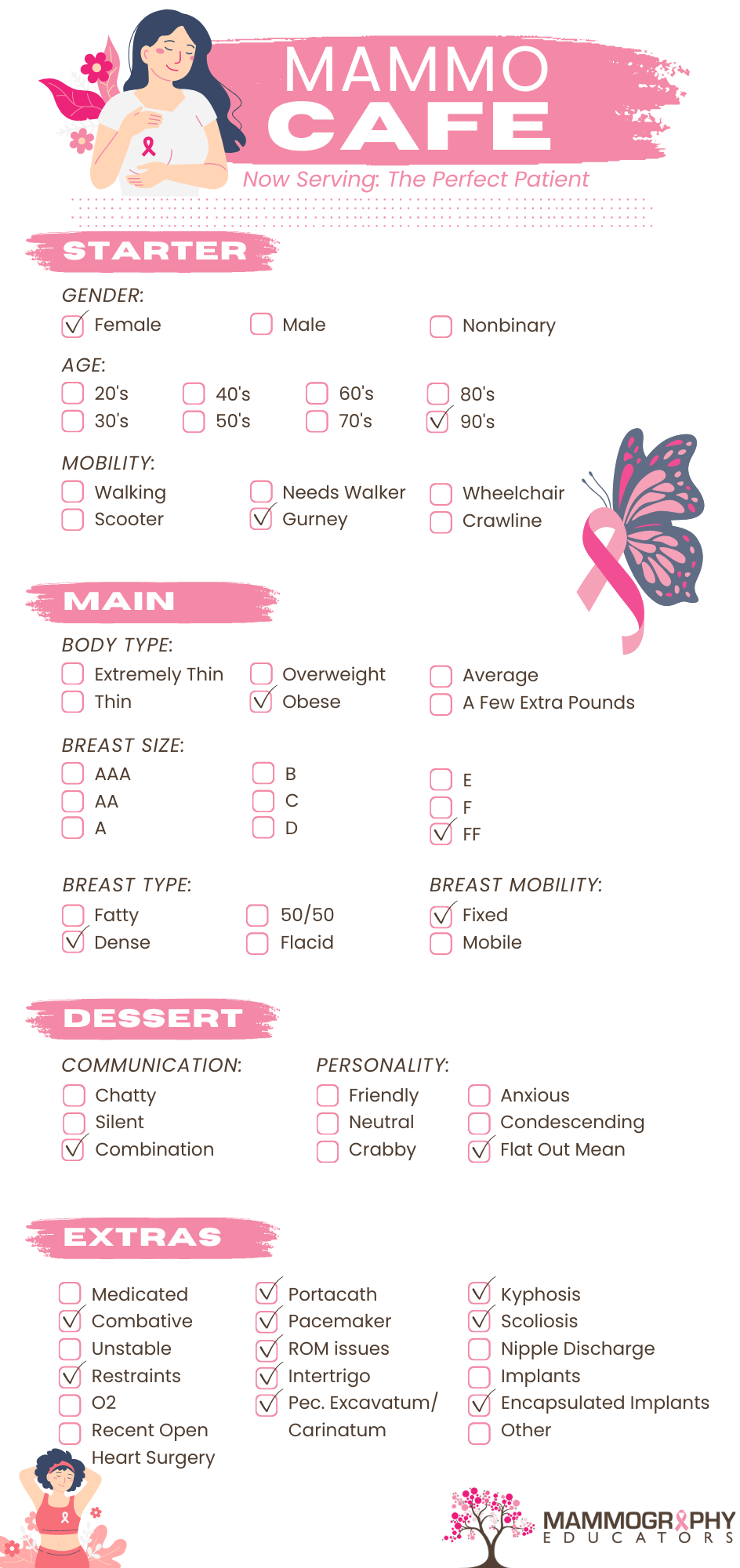
When I started writing this blog, I created a list of challenging patients and situations that were not related specifically to positioning challenges (i.e. frozen shoulder, kyphosis, wheelchair patients, etc) since these were addressed in my previous blog article. This list was based on my personal experience with patients, but then as I talked to other mammographers and read posts in Quality Breast Imagers Facebook Group, I realized that we ALL experience these same challenges and sometimes it is a combination.
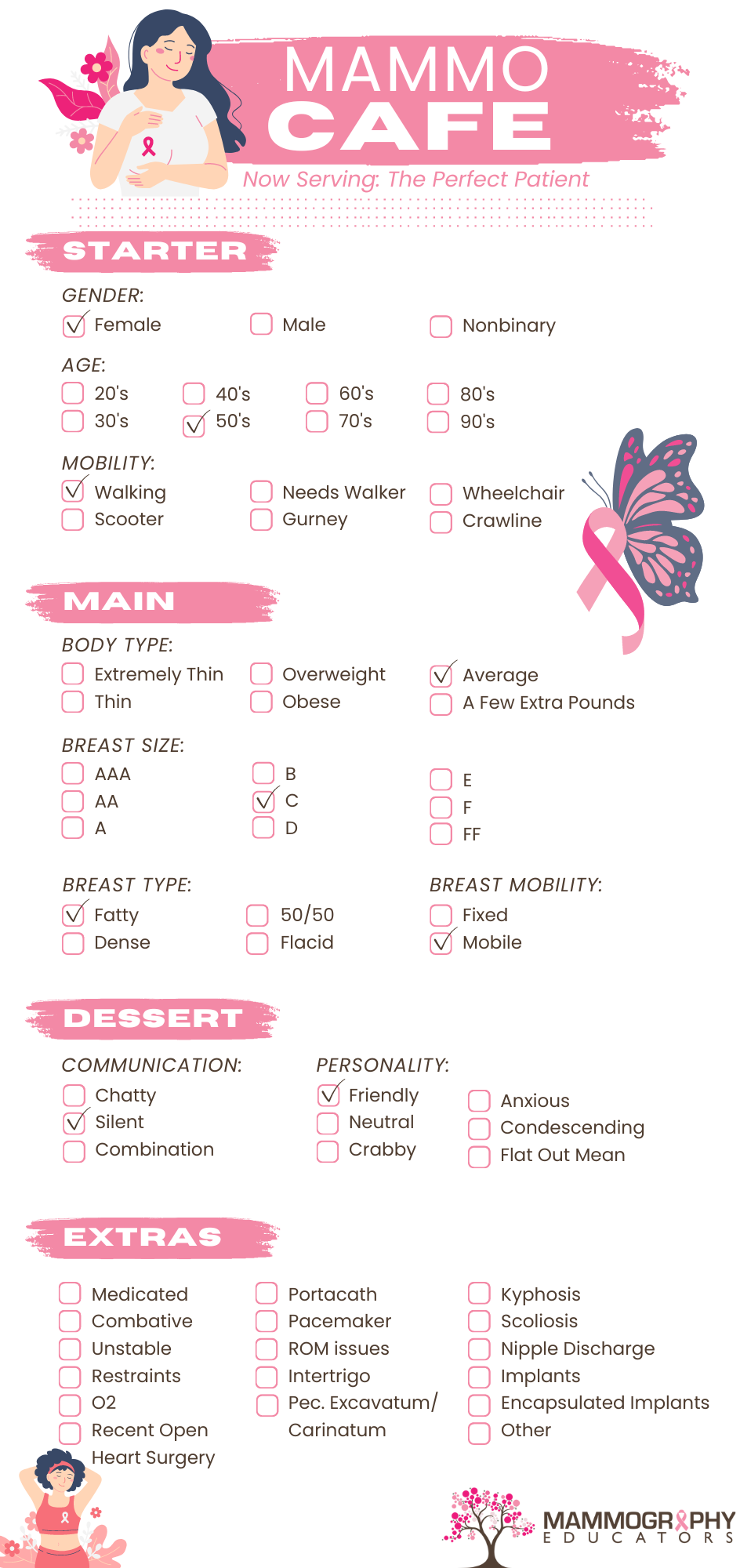
When I was in Las Vegas speaking at a conference several years ago, I saw a restaurant called the Burger Bar. You could order any kind of meat, chicken, bean burger or even lobster! You then got to choose from about 20 different cheeses (from the ‘classic’ American cheese to Brie!), numerous toppings (avocado, onions, bacon, lettuce, shallots, truffles!) and then your condiment(s) of choice: of course, the standards: mustard, mayo, ketchup, but also pesto, guacamole, aioli, hollandaise, etc. You could create your unique ‘combo’! Needless to say, I was all in! 😉 As I was looking over the menu, I thought to myself, “Wouldn’t it be nice if we could ‘order up’ our patients!!” OK, I know, I know. . .but it is never far from my mind, or yours, as I suspect that all mammographers look at people we see/meet as potential mammogram patients! So, check out the Mammo Cafe Menu below!
Order Up!
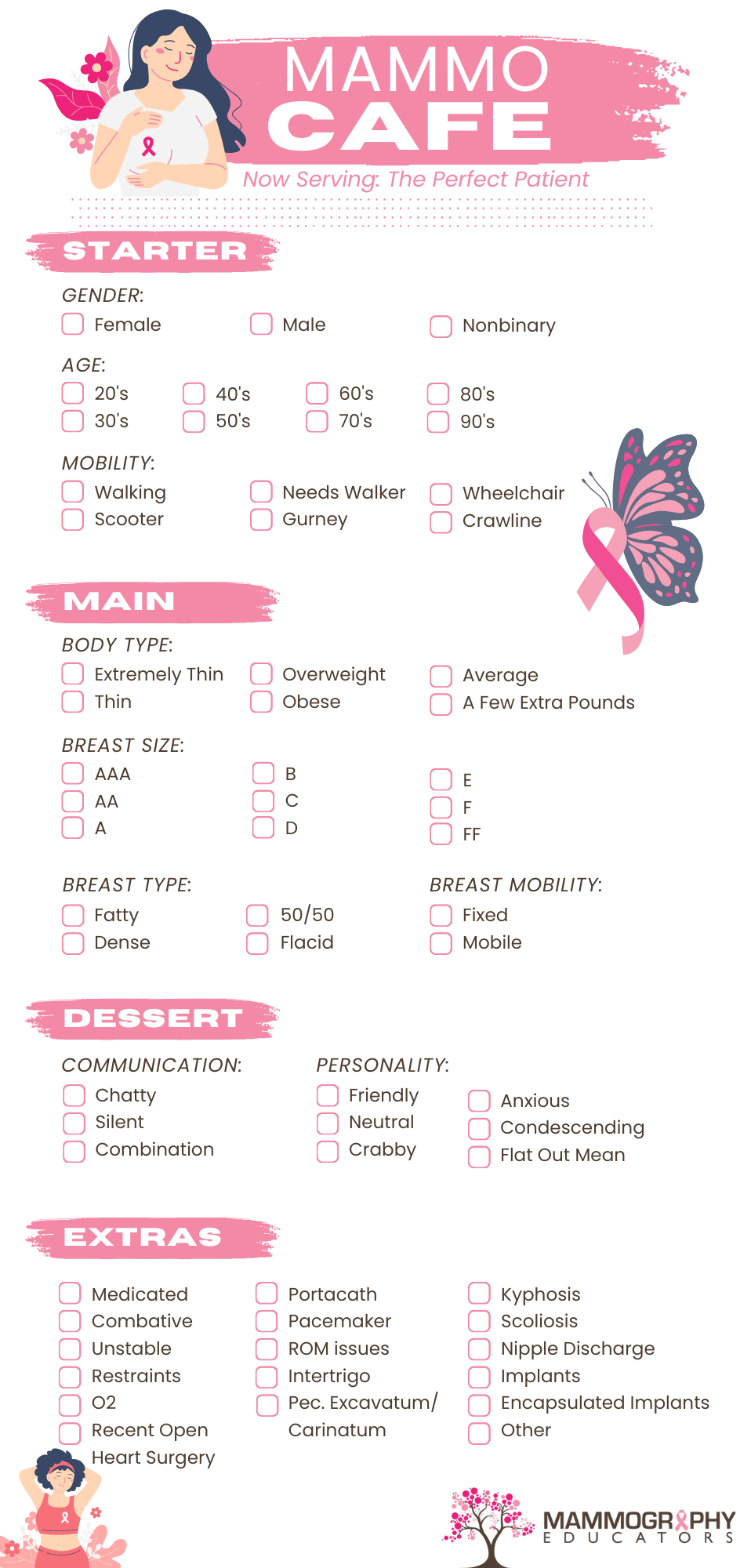
The Dream Patient:
What We're Served:
I plan to go in depth about all these issues in my next book, but wanted to give you some suggestions for improving situations that you can use NOW! As a reminder, these are purely suggestions based on my own experience and the professional recommendations of Dr. Elizabeth Green, PhD who is a licensed psychologist and has provided appropriate and professional suggestions for this article.
GENDER CONSIDERATION
While a patient who is transgender may not have any of the physical or personality traits that other patients exhibit, it is very important to be sensitive to his/her (possibly new) gender identity. This is where gender selection (he/she/her/him/they) is important to establish. Sometimes it may be difficult for the technologist to ascertain as to the patient’s sexual orientation and address her/him/them appropriately. Calling the patient by their first name is usually the best advice. So, ask her/him/them if it is OK to use their first name or is there another way they would like to be addressed. A good resource to become more comfortable and familiar with the use of correct pronouns and gender identify can be found HERE. It is advisable to add a space in your medical history forms where the patient can choose their sexual identification and pronoun of choice. It might also be helpful to have a space where the patient can state how they would like to be addressed.
One of the most important aspects of imaging transgender patients is that you should be following the protocol of your department regarding their imaging. If there is no protocol in place, I suggest following the American College of Radiology ACR Appropriateness Criteria® Transgender Breast Cancer Screening as a guide. It is imperative that a written protocol is approved by all radiologists and all technologists follow said protocol.
As with all other patients, there should never be any judgment on the part of the technologist and each patient should be treated with equal empathy.
CALL-BACKS
TCBs: Technical call backs are easy. Just explain what the problem was and be truthful. For example:
There was some motion or blurring on your images that I was unable to see at the time of your exam, but after the radiologist looked at the pictures, he/she noticed and would like you to come back so we can repeat (insert number) of your images.
After reviewing your images, the radiologist would like you to come back for additional images, so we can get more breast tissue on one of the views.
There’s no reason to lie. You need better images and, while you thought they would be fine (at the time of the exam), the radiologist is the one who makes the final decision as to whether or not images need to be repeated. And aren’t we glad that radiologists are so thorough??!!
Here are some suggestions for Diagnostic Work-up call backs:
- Never call on a Friday.
- Don't call the patient at work.
- If you must leave a message, simply say: "Hi, this is Louise from ABC Breast Center calling for Jolene. Please give me a call at your convenience." Maybe give her the hours at the center, as well as a direct line if possible!
- Never say: "We/the doctor found something on your mammogram that we/they are worried about."
- Do keep the information general: "After reviewing your images, the radiologist would like you to return for some additional pictures (and/or an ultrasound). The reason he/she is asking for this is because many times it is difficult to see through your breast tissue clearly on the initial mammogram, so we do extra pictures and/or an ultrasound to make sure everything is normal for YOU. The next appointment I have available is: . Will that work for you?”
- Answer questions honestly, without scaring the patient! If the patient asks, "Why, what did they see?....Is something wrong?" You can respond by saying, "The reason we do these extra pictures/ultrasound is to be sure that everything is okay and normal for YOU. I can assure you that this is quite routine, as many patients get called back and the vast majority of times, everything is fine."
- Use terminology the patient will understand. Do not get into details by using words like: mass, calcifications, asymmetry, Mag views, spot compression, etc. Most likely they won't know what these things are... Just say "extra pictures on an area that was not clear on the first mammogram".
- Remember that anxiety clouds intake. When patient hears what they think is "bad news," they start to "spin out" in their minds and may assume the worst. This is understandable! So you may have to repeat what you said more than once.
- Leave your phone number with the patient and tell her/him/them to feel free to call you (or a nurse navigator) with any additional questions.
CHALLENGING PERSONALITIES
This is a tough one and I spent a lot of time talking with Dr. Green, our consulting psychologist. We are all used to dealing with many different personality issues…the list is long! But perhaps most challenging is the argumentative and/or condescending patient. Dr. Green suggests that if you feel that the patient is being abusive, you should stop the exam and say to the patient:
"Excuse me. I am going to find another technologist to finish your exam." PERIOD. Then leave and find someone else.