Written by: Belinda Zaparinuk, R.T.(R)(M) BS, CBEC, FNCBC, Breast Imaging Consultant
Quite often you will hear that the primary disadvantage of breast ultrasound is that it's extremely user dependent and takes a long time to perform using handheld transducers. However, in my experience, I have found that to NOT be the case, as long as standardized techniques and protocols are agreed upon and implemented in the breast center. This is my story how, as an administrator in a busy breast center, I completed my goal to create imaging standards for breast ultrasound and improve the efficiency, productivity and continuity of care for the patients and staff.

In 1997, I responded to a Mammography Technologist advertisement in the local newspaper. A couple of weeks later, I received a phone call at 9:00pm from a radiologist who was starting her own breast center. She was passionate and excited about her future plans. This radiologist had just returned from Sweden, where she completed a breast fellowship with Dr. László Tabár, a huge believer in comprehensive breast care.
Dr. Tabár believes that Mammography Technologists are the eyes, the ears and the hands of the radiologist. Therefore, it makes sense to have Mammo Techs performing breast ultrasounds, as well as mammograms. The radiologist who hired me was a great teacher and so was Dr. Tabár. They both were my inspiration to begin training in breast ultrasound.

Since then, I have had the privilege of working at a state-of-the-art facility, which provided the opportunity to excel in my career. Imagine having the funds and support of your facility, to create the breast center of your dreams! The radiologists at this particular center were supportive of Mammography Technologists performing breast ultrasounds. It was agreed upon that our diagnostic technologists would become breast ultrasound certified.
ARRT had a wealth of information and we followed their recommendations. The technologists came up with a plan: we would study together and help each other pass the exam. We were also very fortunate to have two radiologists who were willing to train us and give us feedback during this process. Having the support of your radiologist makes a tremendous difference in creating a solid breast imaging program. Seven of us took the exam, two at a time, until we all passed. (By the way, three techs happened to be over the age of 40... See, you can teach an old dog new tricks!)
Following the exam, we sat down with the radiologists to develop imaging policies and protocols, which was not as difficult as I expected.
We discussed:
• How we would image the whole breast
• When to perform focused and limited ultrasounds
• Call backs
• Six-month follow-ups
• Second look ultrasounds
• How to handle complex breasts (i.e. what to image for documentation and when to refer to CESM, MBI, or MRI).
We also had a plan for male breasts, pregnant patients, and patients under the age of 30. Since each radiologist had a different imaging style; we listened to their rationale. Once the group was in agreement, protocols were developed for each category.
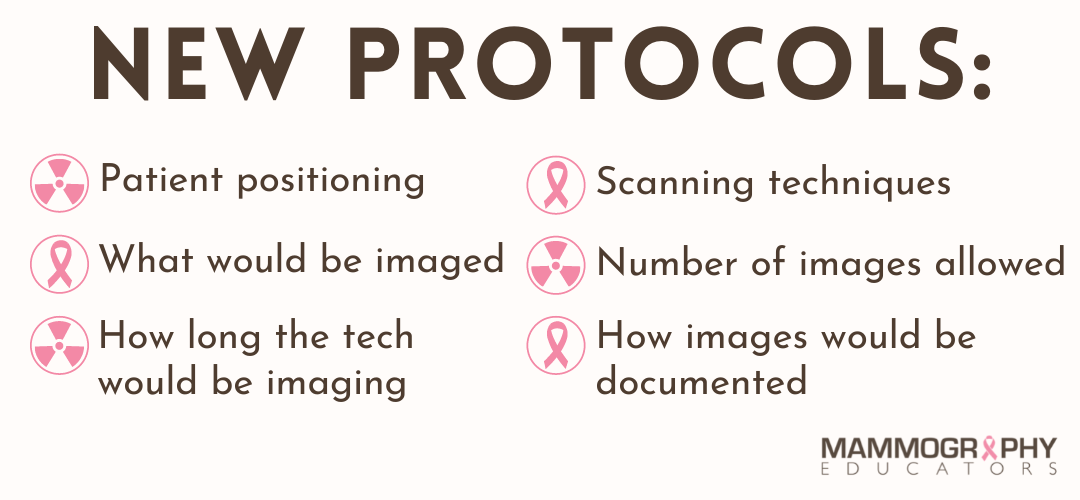
Following the ACR guidelines was helpful in establishing this process. These standardized protocols were not developed overnight, but they were accomplished in time with communication, patience and compromise. A meeting was then held with the technologists, and the new protocols were distributed and an implementation date was given.

The final step, after all the hard work of development and implementation of the protocols, comes compliance and follow-through. We often get excited about starting new things, like "New Year's Resolutions”, but maintaining compliance can become challenging.
Sustaining these new protocols requires diligence, but is achievable. Selecting the correct individual to maintain quality control is the key to the program's success. Weekly or monthly monitoring of the images and adherence to the protocols is also suggested. Reviewing image quality and the outcomes with radiologists and technologist provides a foundation of positive feedback and metrics to measure.
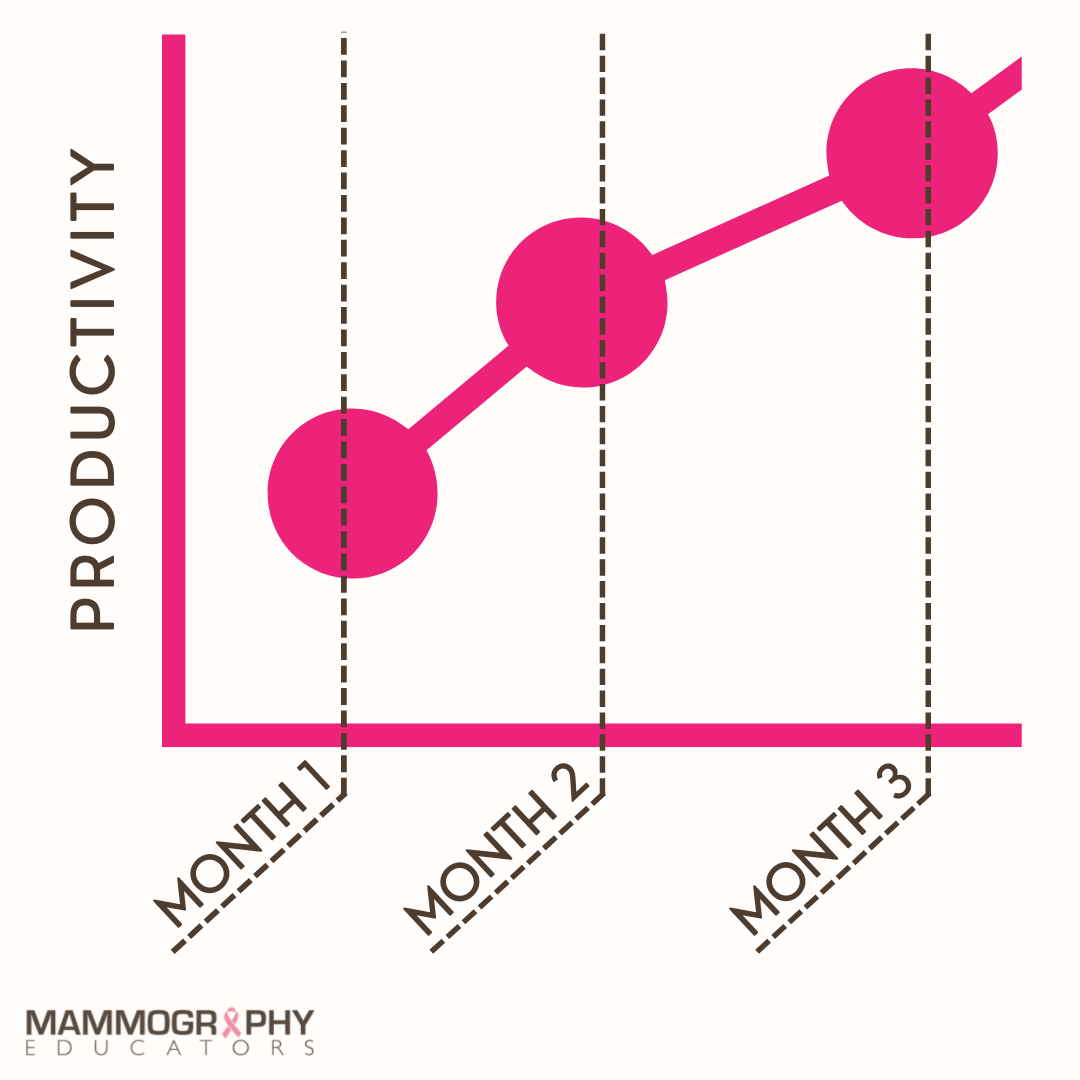
For my facility, we saw a huge change in our breast ultrasound program in about three months. We increased our productivity by 200% from the prior year and we streamlined our scheduling to include ultrasound with each diagnostic exam. This reduced our patient wait time by an average of two to three hours, simply by changing the appointment to a scheduled exam, rather than an add-on patient.
These standardized protocols allowed the technologists to proceed from their mammogram to ultrasound without interrupting the radiologists. We discovered an improved work environment and morale amongst staff, as there was less complaining about waiting on a radiologist or a technologist. Once scanning was completed, the case was presented to the radiologist for review. In our protocol, we had set scanning time to allow the radiologist enough time to come in and scan if needed and to deliver results. This worked seamlessly for our department and both the technologists and radiologists appreciated it.
The biggest improvement seen was in patient satisfaction. Our patients developed a bond with their Mammography Technologist, who was able to see them through to ultrasound and in some cases onto biopsy. Our patient satisfaction scores improved and we consistently maintained monthly scores of 95-100.
Due to the improved continuity of care, our breast cancer detection rate also increased. We eliminated the potential breakdown in communication due to hand off. Everyone was adhering to protocols on scanning the patients. Our ultrasound biopsies increased and stereotactic biopsies decreased, which increased patient comfort and our ability to schedule sooner.
So as you can see from my personal story, breast ultrasound can absolutely be standardized! When implemented appropriately, the process is rewarding for everyone involved: the patient, the technologist and the radiologist! Remembering we are the eyes, the ears and the hands of the radiologist, helps in our crusade of early detection.



