What is Triangulation and Why is it Important?
Triangulation? What the heck does that mean? Do I have to use algebra? Muffins rise? Lead sinks? And why do I need to know this?
These were some of the questions I had when I first heard about triangulation. I was super confused and did not have a clue how to figure this out, except to memorize the sequence of images and determine the direction in which the lesion moved. While that method may work for some, I think it is better to understand why we use an additional view to determine the location of a lesion on a view in which it is not seen.
Triangulation is a process of determining in which area of the breast a lesion will be located based on its known position on two other mammographic images. It is a beneficial method for identifying lesions without relying on one mammographic image. For those who are looking for a deeper understanding of this topic, hopefully this article can help demystify the concept of triangulation.
Imaging Areas of Concern
There are times when an area of concern is imaged on only one of the two standard screening views, the CC and MLO. Prior to the use of DBT, a LM view would frequently be performed to provide additional information for the technologist. If the abnormality is again seen on this projection, it then becomes important to determine the orthogonal (90-degree) location of this area, in order to perform spot compression and perhaps an interventional procedure for a more clear result.
By analyzing the location of the abnormality on the two images where it has been visualized, the general area where it will be located on the other standard screening image can be accurately determined. This information will direct the technologist to select the most appropriate supplementary views to demonstrate the abnormality.
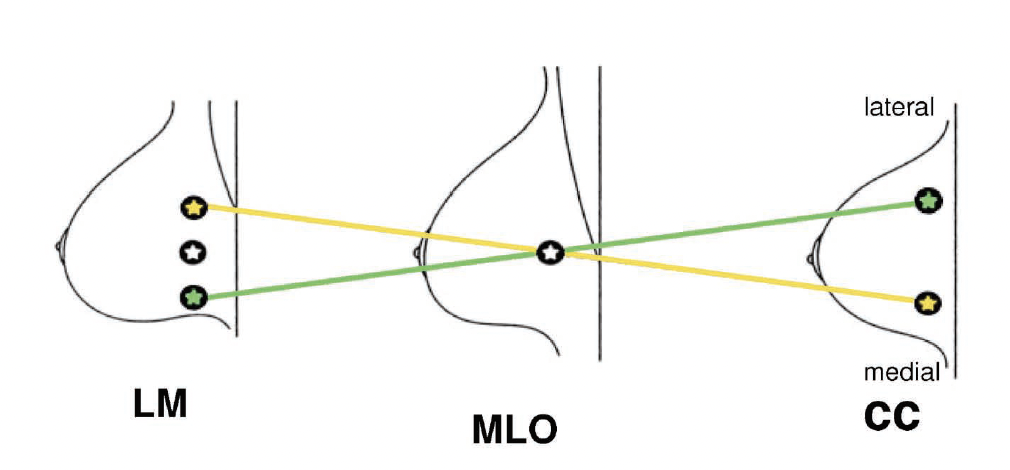
Use the diagram to the right as a reference and follow along with the discussion below.
A lesion that moves DOWN on the lateral view, compared to its location on the MLO view, will be located in the LATERAL part of the breast on the CC projection. In this case, a XCCL should be performed to demonstrate more posterior lateral breast tissue in a CC projection.
Now, when you see a lesion that moves UP on a lateral view, compared to its location on the MLO view, it will be located in the MEDIAL part of the breast on the CC projection. A CV view should then be performed to demonstrate more deep medial breast tissue in a CC projection.
Muffins Rise, Lead Sinks

The moniker “Muffins Rise... Lead Sinks” applies to the comparison as described above. This means M(uffins) rise, or move up, making "M" stand for "Medial". So you would expect to see the lesion in the medial breast by doing a CV view. L(ead) sinks, or moves down, which means L stands for Lateral, so you would expect to see the lesion in the lateral breast by doing an XCCL.
However, it should be noted that if you are comparing the location of the lesion on the MLO to the LM, the opposite will be true. I say this because it has been reported that on state and ARRT exams they ask the question in the opposite manner. For instance, if a lesion moves UP on the MLO compared to the LM, which view should be performed? If you look at the diagram above, the answer would be XCCL. But wait, that doesn’t make sense, does it?
If you memorize ''Muffins Rise, Lead Sinks,'' you would think, Well, if the lesion moved up, then it should be located within the medial breast, i.e.: "Muffins Rise", but in fact, by looking at the diagram and comparing how the lesion moves on the MLO compared to the LM, then you see the correct answer would be that the area of concern would be in the lateral breast, which again is best demonstrated by the XCCL. (If you are about to take the exam, be sure to read the question carefully, as it is very tricky!)
breast triangulation made easy
When you see an area of concern on the MLO view that is not demonstrated on the CC view and you want to:
- Prove it is real versus superimposition of structures
- Locate it on the CC view
The first question that must be answered will be: "Is it real?" This can easily be accomplished through the use of DBT and/or ultrasound. However, you can also answer the question by performing a LM view. If an area of concern was not real, but simply superimposed structures, then it will most likely "disappear". However, if it IS real and persists on the lateral image, compare its location on the LM view to its location on the MLO view. This will help determine where it will be located on the view.
STEP-BY-STEP GUIDE:
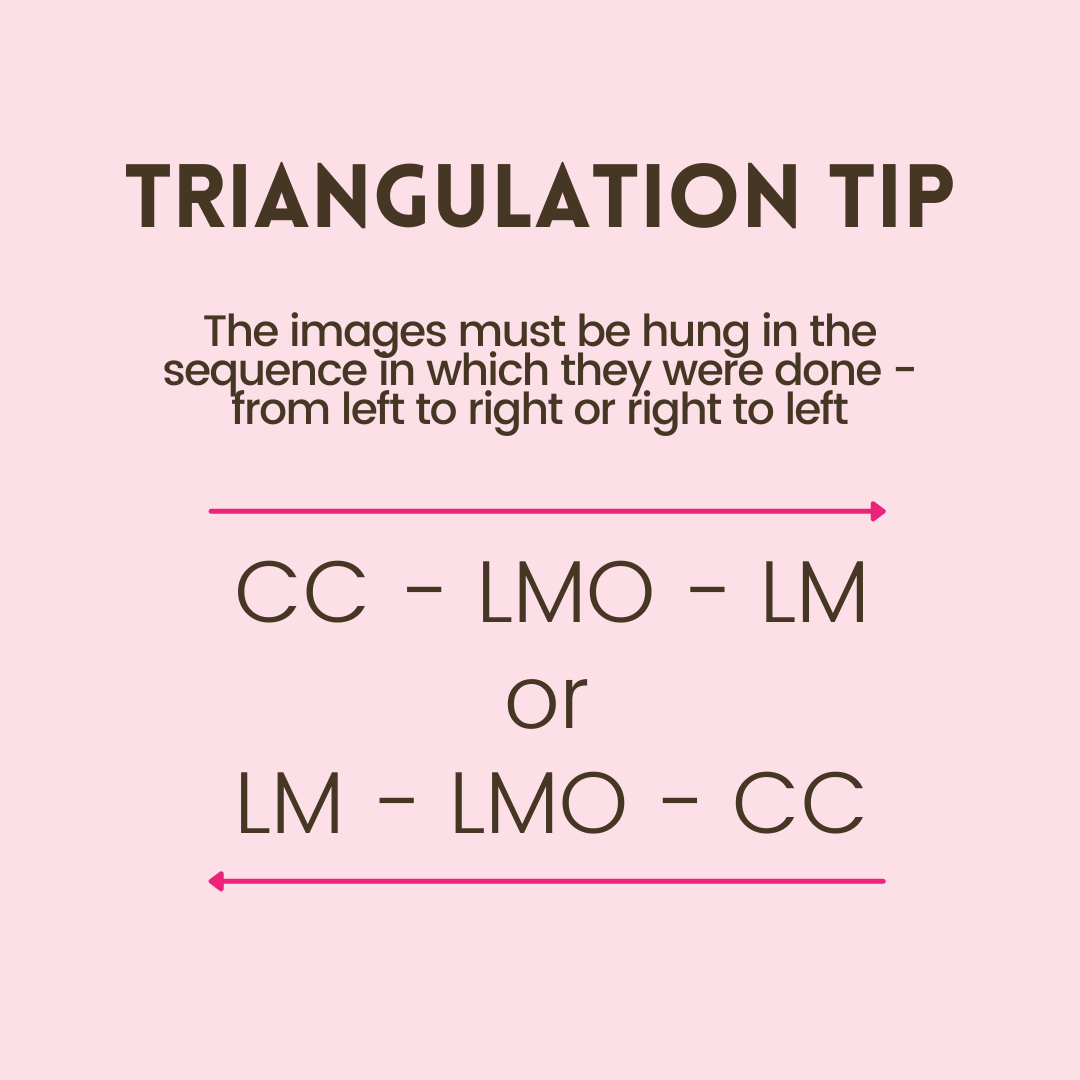
- Line up the images on the monitor in one of the following orders: 1) Left to Right: LM – MLO – CC, or 2) Right to Left: CC - MLO - LM
- Make sure all the nipples are pointing in the same direction, and are at the same level.
- Draw an imaginary line through the area of concern on the LM, then again through the same area of concern seen on the MLO view. Extend this line into the CC view and it will “point” to the area where the lesion should be located on the CC view. Knowing the general location of the abnormality allows you to focus on additional views that will demonstrate this area more thoroughly. (For example: XCCL for lateral lesions and CV for medial lesion.)
I hope that both Positioning Dynamite TNT Part 1 and Part 2 (this article) helped you better understand the use and performance of these techniques. With proper education of triangulation and practice, you'll find it's not so scary after all!